Nature:儿童室管膜瘤与RELA基因密切相关
2014-02-21 佚名 生物通
St. Jude儿童研究医院-华盛顿大学儿科癌症基因组项目的科学家们,鉴别出了迄今为止报道的室管膜瘤(ependymoma)最常见的遗传变异,并证实这一变异驱动了肿瘤形成。相关研究发表在2月19日的《自然》(Nature)杂志上。【原文下载】 这些研究结果为开展新的研究以改善这一第三大最常见儿童脑瘤的诊断和治疗奠定了基础。此外,新研究也将有助于了解和干预治疗包括成人肿瘤在内的其他癌症。 新
St. Jude儿童研究医院-华盛顿大学儿科癌症基因组项目的科学家们,鉴别出了迄今为止报道的室管膜瘤(ependymoma)最常见的遗传变异,并证实这一变异驱动了肿瘤形成。相关研究发表在2月19日的《自然》(Nature)杂志上。【原文下载】
这些研究结果为开展新的研究以改善这一第三大最常见儿童脑瘤的诊断和治疗奠定了基础。此外,新研究也将有助于了解和干预治疗包括成人肿瘤在内的其他癌症。
新发现的遗传变异与一个叫做RELA的基因有关。RELA基因在调控炎症的细胞信号系统——NF-κB信号通路中起着极其重要的作用。研究人员很久以前就认识到在许多的成人肿瘤中NF-κB信号通路被不恰当地开启。这项研究是科学家们第一次在脑癌中发现存在于这一信号通路中心部分的一个基因变异。
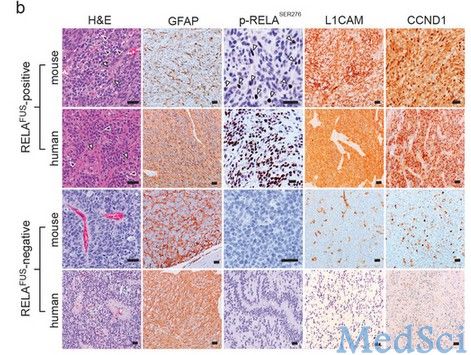
新研究发现,70%前脑有室管膜瘤的年轻患者都携带有RELA变异以及少数其他的遗传变异。在大脑其他区域的室管膜瘤中则未发现有这种变异。
论文的共同通讯作者、St. Jude综合癌症中心主任Richard Gilbertson博士说:“在这项研究中我们第一次证实,存在于NF-κB信号通路中心的一个频发突变足以将正常脑细胞转变为癌细胞,并驱动肿瘤形成。这应该有助于我们了解异常NF-κB活性驱动癌症的机制,以及开发出新的治疗方法来阻断这一活性。”
这一变异使得在一个称之为易位的过程中RELA与另一基因C11orf95发生融合。易位导致生成的异常蛋白在小鼠体内快速地引发了致命性的脑瘤。这些肿瘤与人类室管膜瘤相似。 论文共同作者、华盛顿大学医学院基因组研究所所长Richard K. Wilson说:“这是一个令人兴奋的研究发现,其不仅让我们了解了罕见且尤具有破坏性的一种儿童脑癌的生物学,并且也有助于我们了解如何可以有效地治疗它。”
St. Jude现正领导一项国际研究一确定C11orf95-RELA易位是否可能有助于预测室管膜瘤患者的结局。St. Jude还开发了一种测试来鉴别携带这种易位的肿瘤。共同通讯作者、St. Jude病理系主任负责领导这项工作。
St. Jude研究人员开发的一种名为CICERO的分析工具在鉴别出这一易位中起关键作用。共同通讯作者、St. Jude计算生物学系准成员Jinghui Zhang博士领导研究小组开发了CICERO。
研究人员通过筛查包含41名年轻室管膜瘤患者肿瘤完整遗传密码和正常DNA的2460亿个遗传信息片段发现了这一易位。此外,研究人员还研究了77个室管膜瘤的RNA。通过测序DNA和RNA,科学家们可以看到哪些基因被开启并在形成诸如RELA易位一类的异常产物。
利用CICERO,研究人员发现了一些RNA异常由此引导他们揭示出了C11orf95-RELA易位。当定位在11号染色体上的C11orf95和RELA基因发生断裂并错误地重新组装到一起时便生成了这一融合基因。
这是迄今为止报道的、在脑肿瘤中最常发生的易位之一。研究中的41个形成于前脑的室管膜瘤有29个存在这种易位,并生成了RELA融合蛋白。“发现这种变异导致了一些异常的蛋白质,这一事实为我们提供了一个潜在的新治疗靶点,这对于室管膜瘤具有重要的意义,”Gilbertson说。
研究人员现正致力于了解这种融合蛋白导致癌症的机制。有证据表明,C11orf95通过改变RELA穿过细胞执行正常功能的方式发挥了关键的作用。研究人员还发现一些涉及其他基因的易位似乎也驱动了室管膜瘤。
原始出处:
Matthew Parker,Kumarasamypet M. Mohankumar,Chandanamali Punchihewa,Ricardo Weinlich,James D. Dalton, Yongjin Li,Ryan Lee, Ruth G. Tatevossian,Timothy N.Phoenix,RadhikaThiruvenkatam, Elsie White,Bo Tang,Wilda Orisme,Kirti Gupta,Michael Rusch,Xiang Chen,Yuxin Li,Panduka Nagahawhatte,Erin Hedlund,David Finkelstein,Gang Wu,Sheila Shurtleff,John Easton,Kristy Boggs,Donald Yergeau,Bhavin Vadodaria,Heather L. Mulder,Jared Becksford,Pankaj Gupta,Robert Huether,Jing Ma,Guangchun Song,Amar Gajjar,Thomas Merchant,Frederick Boop,Amy A. Smith,Li Ding,Charles Lu,Kerri Ochoa,David Zhao,Robert S. Fulton,Lucinda L. Fulton,Elaine R. Mardis,Richard K. Wilson,James R.Downing,Douglas R. Green,Jinghui Zhang,David W. Ellison& Richard J. Gilbertson.C11orf95–RELA fusions drive oncogenic NF-κB signalling in ependymoma.Nature 19 February 2014 doi:10.1038/nature13109【原文下载】
Extended Data Figure 7: Analysis of C11orf95–RELA translocation and expression in formalin-fixed paraffin-embedded human and mouse ependymoma.Nature (2014) doi:10.1038/nature13109
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#Nat#
38
#管膜瘤#
46
#室管膜瘤#
31
#室管膜瘤#
31