Brit J Cancer:GAS5肿瘤抑制因子lncRNA功能丧失研究
2018-11-09 AlexYang MedSci原创
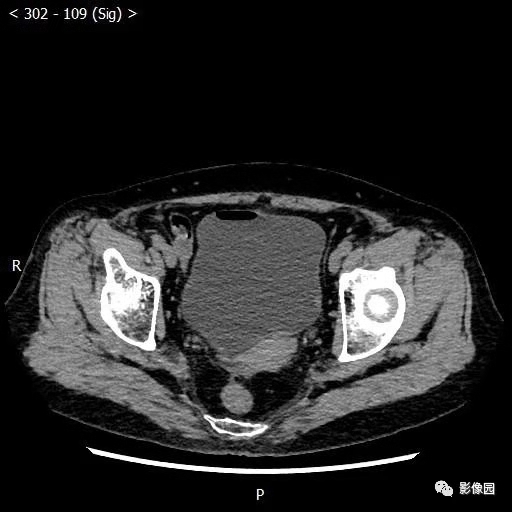
膀胱癌(BlCa)遗传异质性和个性化预后的缺乏导致了患者治疗结果的高度可变性。最近,有研究人员分析了GAS5肿瘤抑制因子lncRNA在改善BlCa预后中的作用。研究人员在一个176名患者组成的筛选群体中对GAS5进行了定量,并将Hedegaard et al.(2016)文章中的476名和TCGA临时性群体(n=413)作为鉴定群体。研究人员还使用复发和恶化对NMIBC进行了生存分析,并利用死亡数
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#肿瘤抑制因子#
62
#肿瘤抑制#
39
#CRN#
35
#lncRNA#
37
#抑制因子#
38
学习了,谢谢作者分享!
52
#GAS#
26
了解一下,谢谢分享!
66