JAMA Oncol:每月补充高剂量维生素D真的可以降低患癌风险么??
2018-07-24 肿瘤资讯编辑部 肿瘤资讯
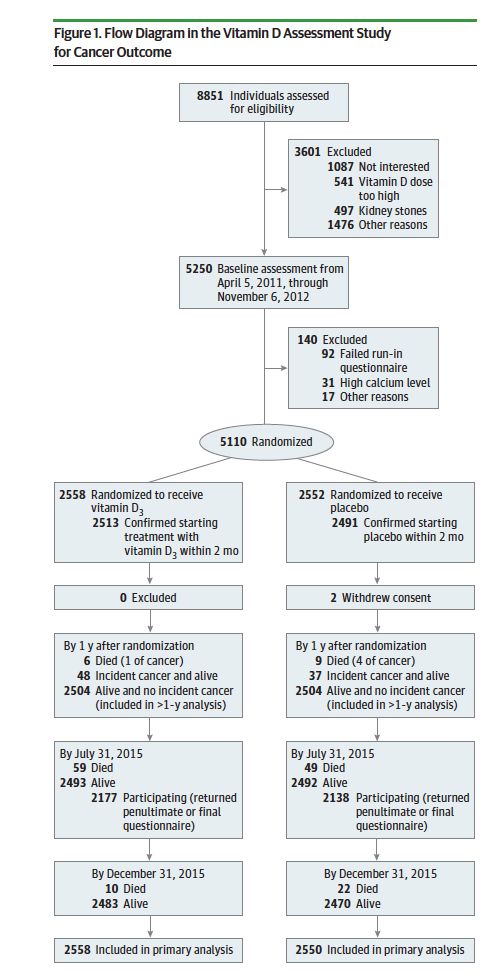
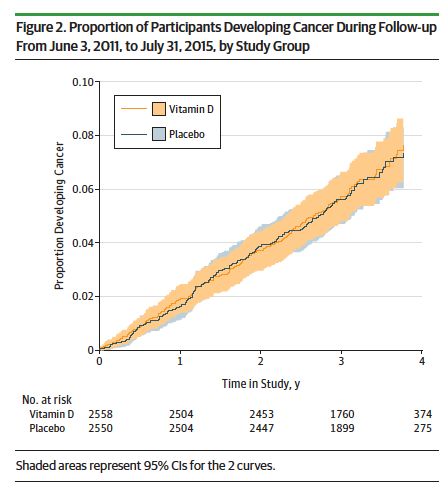
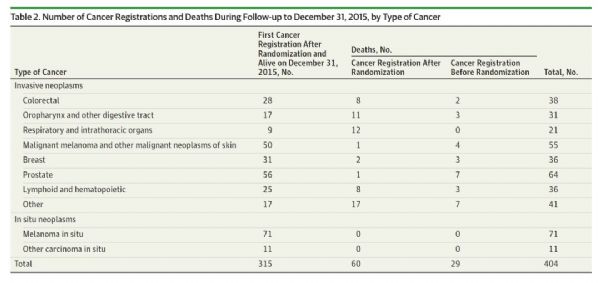
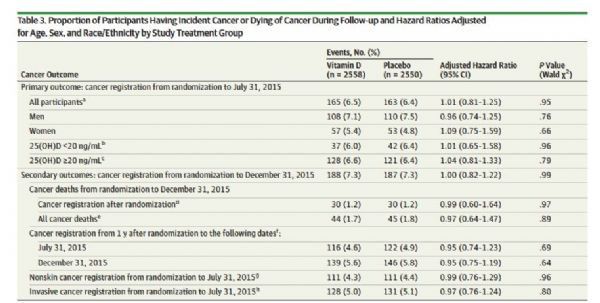
既往研究提示维生素D(VitD)可能可以降低患癌风险,目前关于VitD补充与癌症发病风险的关系,尚无定论。近期发表在《JAMA Oncology》杂志的研究,对一项大型社区随机对照研究进行了事后分析,以探索VitD补充是否可以降低癌症发病风险。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#癌风险#
26
#Oncol#
28
#高剂量#
30
学习了
65
已学习
55
#患癌风险#
33
#患癌#
28
学习了
50