Pediatrics:注射疫苗帮助儿童战胜肺炎
2014-12-14 MedSci MedSci原创译
肺炎链球菌是肺炎的主要致病菌,肺炎每年引起超过1百万的儿童死亡。而鼻窦炎也能导致儿童肺炎,甚至引起眼睛和颅内感染。尽管肺炎链球菌疫苗(PCV)可以有效抵御肺炎链球菌的侵入,但是它对能否有效防止肺炎还是个未知数。为了研究PCV疫苗与肺炎的关系,瑞典公共健康机构的Ann Lindstrand医生比较了PCV7和PCV13疫苗接种前后鼻窦炎、肺炎和脓胸的住院率。研究对象为2003-2012年瑞典斯德哥尔
肺炎链球菌是肺炎的主要致病菌,肺炎每年引起超过1百万的儿童死亡。而鼻窦炎也能导致儿童肺炎,甚至引起眼睛和颅内感染。尽管肺炎链球菌疫苗(PCV)可以有效抵御肺炎链球菌的侵入,但是它对能否有效防止肺炎还是个未知数。
为了研究PCV疫苗与肺炎的关系,瑞典公共健康机构的Ann Lindstrand医生比较了PCV7和PCV13疫苗接种前后鼻窦炎、肺炎和脓胸的住院率。
研究对象为2003-2012年瑞典斯德哥尔摩地区0-18岁因鼻窦炎、肺炎或脓胸住院的儿童。研究者根据这些儿童的住院病历系统展开以人群为基础的研究。将病例分为2003年7月-2007年7月组以及2008年6月至2012年6月组,排除PCV疫苗上市的那一年。研究内容包括趋势分析、发病率和比值比。
结果发现,PCV疫苗接种后,0-2岁患儿的鼻窦炎住院率从每十万名儿童70人下降到24人,0-2岁患儿的肺炎住院率从每十万名儿童450人下降到366人,2-5岁患儿的肺炎住院率从每十万名儿童250人下降到212人。脓胸住院率下降并不显著。趋势分析的结果显示(图1),0-2岁患儿注射疫苗之前肺炎住院率上升,0-5岁患儿注射疫苗之后鼻窦炎和肺炎住院率显著下降。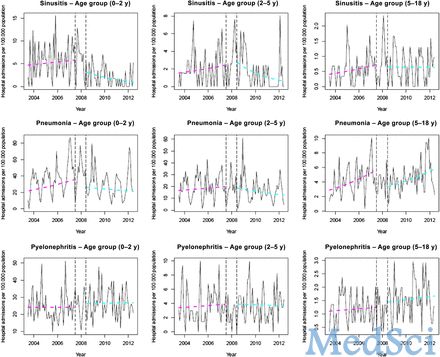
图1 每10万人口住院率趋势分析
研究表明,相比于疫苗注射前的4年时间,PCV7和PCV13疫苗注射后的4年时间内,0-2岁患儿鼻窦炎住院风险下降了66%,肺炎住院风险下降了19%。换句话说,PCV能够有效防止0-2岁儿童患上肺炎。
原始出处:
Lindstrand, A., et al., Sinusitis and pneumonia hospitalization after introduction of pneumococcal conjugate vaccine. Pediatrics, 2014. 134(6): p. e1528-36.

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








有意思
128
有这种效果吗?
165
#DIA#
38
#Pediatric#
35
#PE#
34