Stroke:取栓后,血压变异和不良预后息息相关
2021-08-25 Freeman MedSci原创
成功再灌注后的高频血压波动,可能是有害的,并与神经系统恢复的可能性降低和有利的功能结果有关
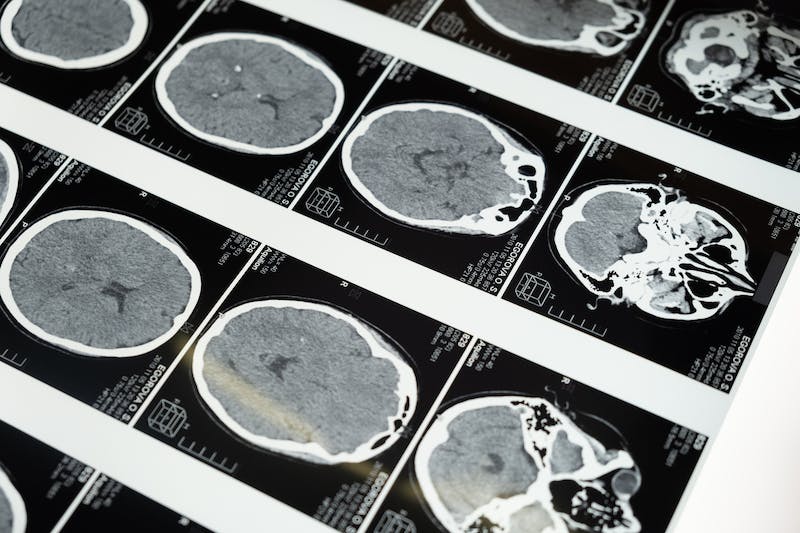
在血管内卒中治疗(EVT)后的最初几个小时内,血压(BP)升高的患者发生出血性转变的风险增加,结果更差。
由于脑部自动调节功能受损,容易造成脑部低灌注或高灌注,避免血管重建后血压大幅波动与治疗高血压水平同样重要。
传统的血压变异性测量通常需要24小时的血压监测,限制了其对临床决策的作用。
藉此,Pedro Castro等人, 利用频谱分析从5分钟的搏动记录中评估血压变异性,并评估其预测早期神经系统恢复和长期功能结果的能力。
他们对146名成功接受血管内治疗的前循环缺血性卒中患者,进行了一项前瞻性研究。对5分钟的逐次血压记录进行频谱分析,以量化血压变异性。
临床结局:包括最初的临床反应和90天后的改良Rankin量表。
他们发现:高频率的血压变异性增加与90天时的功能障碍独立相关(调整后的几率aOR=1.85[95%CI,1.07-3.25],P=0.03;
调整基线严重程度后,较高的正常化高频率(aOR=1.85[95%CI,1.07-3.25],P=0.03)和LF/HF(低/高频率比值)比率(aOR=0.67[95%CI,0.46-0.92],P=0.02)与不良功能结局独立相关。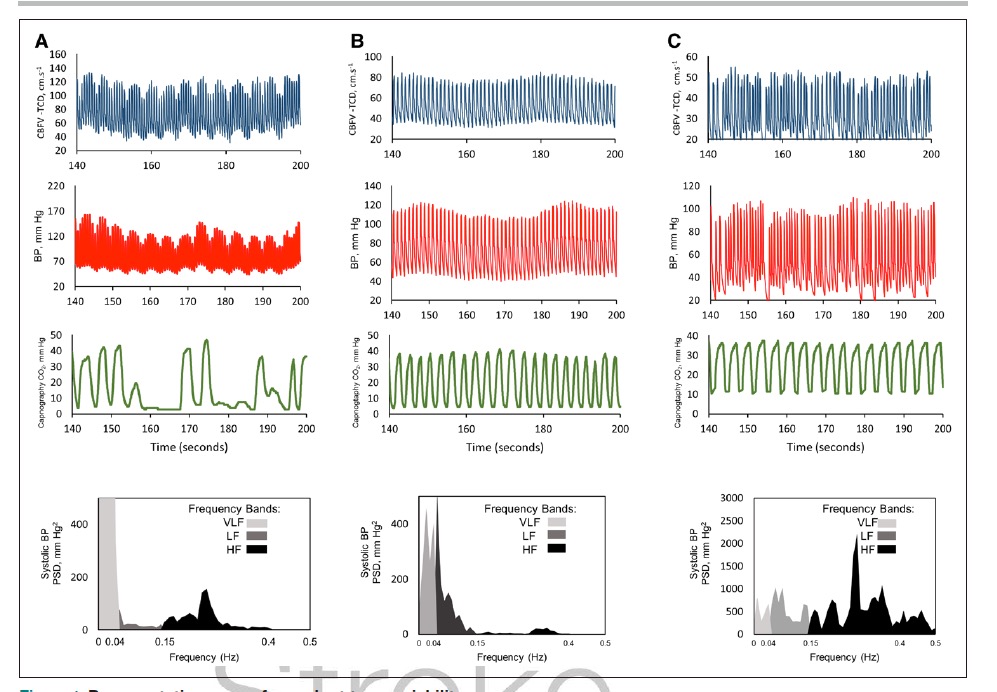
较高的正常化HF功率和较低的LF/HF比率也降低了神经系统恢复的可能性(aOR=0.62[95%CI,0.44-0.91],P=0.01;aOR=1.37[95%CI,1.03-1.87],P=0.04)
这个研究的重要意义在于发现了:成功再灌注后的高频血压波动,可能是有害的,并与神经系统恢复的可能性降低和有利的功能结果有关。快速评估再灌注后整个时期的血压变异性是可行的,并可能允许更个性化的血压管理。
原文出处:
Castro P, Ferreira F, Nguyen CK, et al. Rapid Assessment of Blood Pressure Variability and Outcome After Successful Thrombectomy. Stroke. Published online July 27, 2021. doi:10.1161/STROKEAHA.121.034291
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言


















#不良预后#
0
#变异#
27
#取栓#
48
学习了
53