FDA授予Enhertu在肺癌中的优先审查权
2022-04-22 Allan MedSci原创
如果获得批准,这将是 Enhertu 的第三种肿瘤适应症。
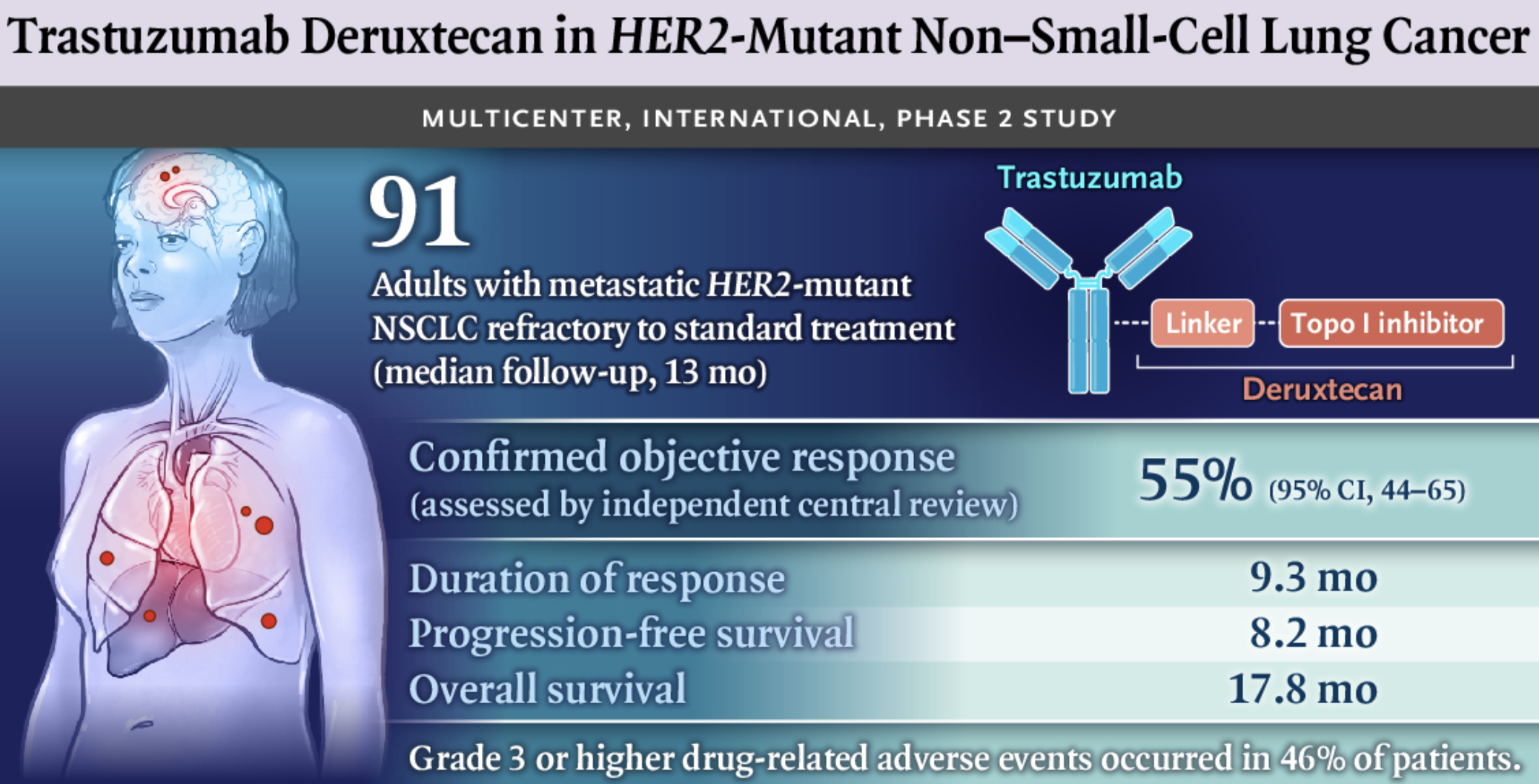
阿斯利康(AstraZeneca)和第一三共(Daiichi Sankyo)近日宣布,美国食品和药品监督管理局(FDA)已批准一项寻求扩大抗体药物偶联物(ADC)Enhertu(fam-trastuzumab deruxtecan-nxki)适应症以包括肺癌的文件的优先审查权。两家公司希望 Enhertu 用于治疗接受过全身治疗的 HER2 突变、不可切除或转移性非小细胞肺癌(NSCLC)患者。
该申请基于关键 II 期 DESTINY-Lung01 试验的数据,其中靶向 HER2 的 ADC 显示出 54.9% 的缓解率。在去年 9 月欧洲医学肿瘤学会(ESMO)会议上公布的其他结果中,经过一年多的随访,Enhertu 组患者的中位无进展生存期(PFS)为 8.2 个月,中位总生存期(OS)为 17.8 个月。
AstraZeneca 肿瘤学研发负责人 Susan Galbraith 表示:“Enhertu 有可能成为这一患者群体的新标准治疗方法。”两家公司指出,目前尚无针对 HER2 突变 NSCLC 的 HER2 靶向疗法。
如果获得批准,这将是 Enhertu 的第三种肿瘤适应症。该药物于 2019 年首次获得加速批准用于 HER2 阳性不可切除或转移性乳腺癌,于2021年获得 FDA 批准用于先前治疗的 HER2 阳性局部晚期或转移性胃癌。
人表皮生长因子受体2(HER2)是乳腺癌重要的驱动基因和预后指标,也是抗HER2药物治疗的主要预测指标。HER2阳性乳腺癌临床占比20%左右。近年来,针对HER2的生物靶向药物成为治疗乳腺癌的重要突破。抗HER2药物在HER2阳性乳腺癌的治疗中取得良好效果,改变了临床实践。Enhertu(fam-trastuzumab deruxtecan-nxki)的设计通过一种4肽链接子将靶向HER2的人源化单克隆抗体trastuzumab与一种新型拓扑异构酶1抑制剂exatecan衍生物链接在一起,可靶向递送细胞毒制剂至癌细胞内,与通常的化疗相比,可减少细胞毒制剂的全身暴露,能够特异性地杀灭癌细胞。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Enhertu#
54
#优先审查#
45
***#学习#
55
#房颤#好
104
学习
73