NEJM:稳定型胸痛患者CT或有创冠状动脉造影的比较
2022-04-28 MedSci原创 MedSci原创
对于稳定型胸痛和中等的阻塞性冠状动脉疾病预测概率而接受ICA的患者,CT组和ICA组发生主要不良心血管事件的风险相似。采用CT诊断策略时,主要手术相关并发症的发生率较低。
近日,顶级医学期刊NEJM上发表了一篇研究文章,研究人员进行了一项实用的随机试验,以比较CT和ICA作为初始诊断影像策略,以指导转诊到26个欧洲中心之一进行ICA的阻塞性冠状动脉疾病的稳定型胸痛患者。该研究的主要结局为3.5年的主要不良心血管事件(心血管死亡、非致死性心肌梗死或非致死性卒中),主要的次要结局是手术相关并发症和心绞痛。
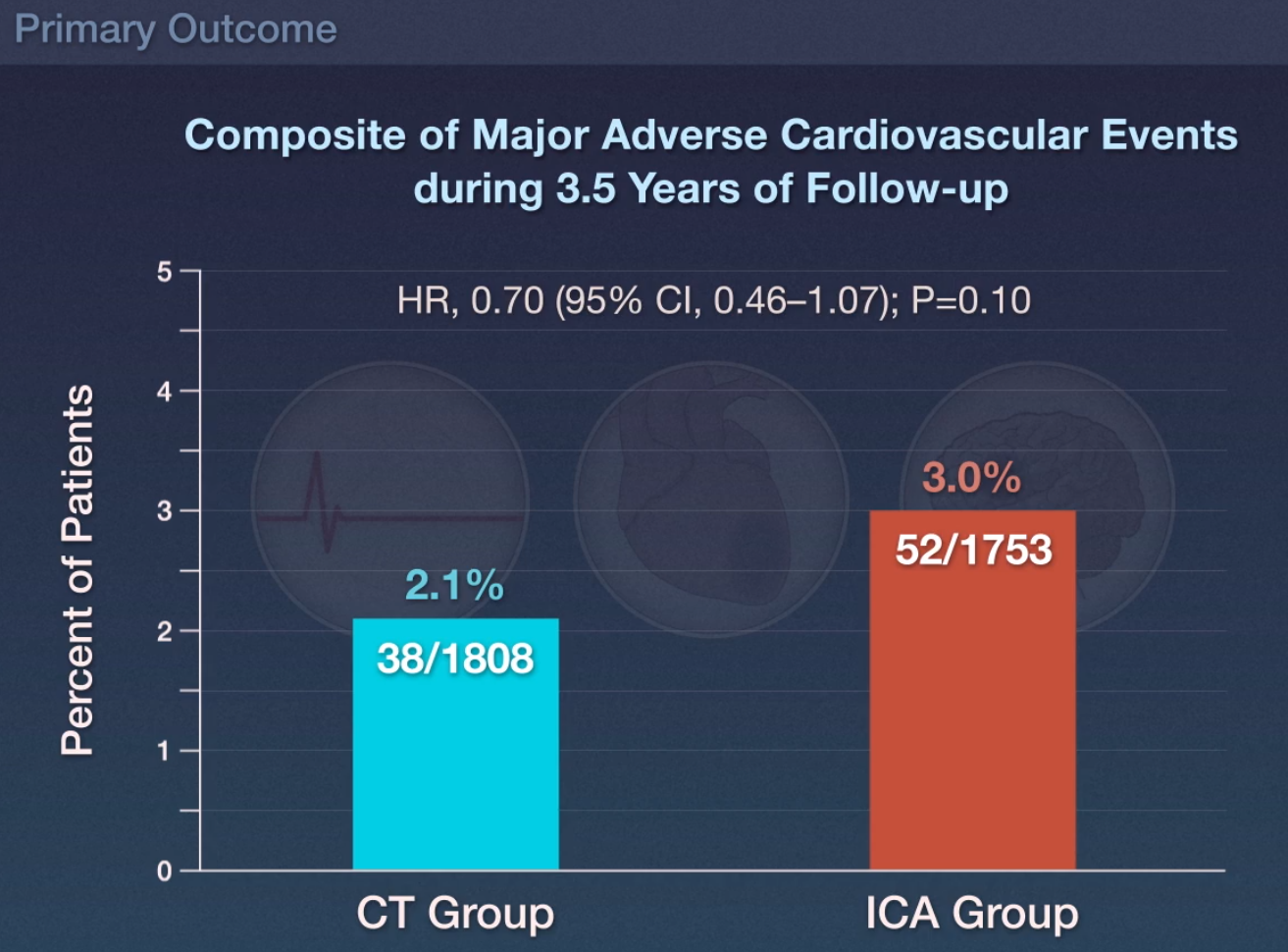
在3561例患者(56.2%为女性)中,有3523例(98.9%)完成了随访。1808例CT组患者中有38例(2.1%)发生主要不良心血管事件,1753例ICA组患者中有52例(3.0%)发生主要不良心血管事件(风险比为0.70;95%置信区间[CI]为0.46~1.07;P = 0.10)。
进一步研究发现,CT组有9例(0.5%)发生重大手术相关并发症,ICA组有33例(1.9%)发生重大手术相关并发症(风险比为0.26;95%CI为0.13~0.55)。在随访的最后4周,8.8%的CT组患者发生心绞痛,7.5%的ICA组患者发生心绞痛(比值比为1.17;95%CI为0.92~1.48)。
由此可见,对于稳定型胸痛和中等的阻塞性冠状动脉疾病预测概率而接受ICA的患者,CT组和ICA组发生主要不良心血管事件的风险相似。采用CT诊断策略时,主要手术相关并发症的发生率较低。
原始出处:
The DISCHARGE Trial Group.et al.CT or Invasive Coronary Angiography in Stable Chest Pain.NEJM.2022.https://www.nejm.org/doi/full/10.1056/NEJMoa2200963
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#稳定型#
35
很不错的研究发现,学习了,非常感谢
45
#冠状动脉造影#
33
#造影#
47
NEJM上果然牛,感谢梅斯更新及时
43