强生召回部分问题球囊扩张导管
2012-07-17 中国网 www.china.com.cn
美国 FDA网站上将“Dura Star” 和 “Fire Star”球囊导管召回事件定为最严重的“一级召回”。 中国网7月13日讯(记者 刘永晓 马艺文)7月12日,跨国制药企业强生公司再次出现召回事件:由于可能会出现“缓慢收缩”或“无法收缩”的问题,强生宣布召回Cordis公司生产的球囊扩张导管(商品Fire Star),涉及产品批号为15437344。 从国家药监局官方微博“中国
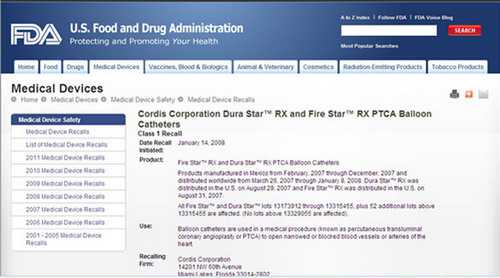
美国 FDA网站上将“Dura Star” 和 “Fire Star”球囊导管召回事件定为最严重的“一级召回”。
中国网7月13日讯(记者 刘永晓 马艺文)7月12日,跨国制药企业强生公司再次出现召回事件:由于可能会出现“缓慢收缩”或“无法收缩”的问题,强生宣布召回Cordis公司生产的球囊扩张导管(商品Fire Star),涉及产品批号为15437344。
从国家药监局官方微博“中国药监”上披露的消息获悉,宣布召回的该款产品在中国共有118盒,其中销售86盒,库存32盒。
这次召回事件不同于以往数十次“和中国市场无关”的召回,这是强生公司主动在中国国内召回所属产品。
“无法收缩”的导管手术后拔不出
球囊扩张导管,是一种在心脏介入手术中普遍应用的医疗用品。它的主要作用是用于支撑冠状动脉的狭窄部分,来支持心脏手术的正常进行。
“基本上每一例心脏介入手术都要用到球囊扩张导管,手术之后再拔出来。”阜外心血管病医院心血管博士后杨进刚告诉中国网财经中心记者,如果出现“缓慢收缩”或者“无法收缩”的问题,放入患者血管中的球囊导管无法拔出来,强行拔出就会造成心内膜损伤。
“本来直径只有1mm的血管,通过球囊扩张导管支撑到3mm,如果无法收缩,拔出来的时候血管都要被撑到3mm的程度,心脏动脉就会损伤,心率发生改变,严重的可能会导致心梗。”杨进刚说。
但由于临床使用比较普遍,杨进刚认为可能是这个品牌的某一批次或者某一型号的球囊扩张导管出现了问题。
2008年初曾全球召回 当年6月进入中国
此次召回的强生公司“Fire Star”球囊扩张导管,是在2008年6月获批进入中国市场的,但该产品在2008年1月14日久被美国FDA通告“一级召回”。
中国网财经中心记者在美国食品和药品监督管理局官方网站(http://www.fda.gov)上找到了召回的详细信息。
在2008年1月14日的公告中,强生在美国宣布召回“Dura Star” 和 “Fire Star”球囊导管,美国 FDA网站上将该事件定为最严重的“一级召回”。当年召回的原因就是“缓慢收缩”或“无法收缩”。
四年前在美国出现的同样问题,四年后在中国再次出现。对此,中国网财经中心记者致电强生公司媒体服务部经理蒋柯时,对方否认了强生同类产品曾被FDA通告。
强生称未使用的55盒导管产品已被管控
截稿前,中国网财经中心收到了强生公司对于此次召回的书面进展说明:强生(中国)医疗器材有限公司于6月13日完成该批次产品相关的医院和经销商的通知工作,并于6月18日上报上海市食品药品监督管理局。
据悉,该批次产品的召回只涉及亚洲市场。在中国,共涉及到118盒该产品,截止到目前为止,未使用的55盒产品全部在强生(中国)医疗器材有限公司的管控之下。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#球囊扩张#
30
#扩张#
36
#球囊扩张导管#
27
#强生#
35
#球囊#
34
#召回#
31