Front Oncol:仑伐替尼(Lenvatinib)单药或联合PD-1抑制剂治疗中国晚期肝癌患者的疗效和安全性
2021-12-17 yd2015 MedSci原创
仑伐替尼目前被批准用于晚期肝癌患者的一线治疗。我们也知道PD-1抑制剂也被用于晚期肝癌患者。那仑伐替尼单药或联合PD-1抑制剂治疗中国晚期肝癌患者的真实世界疗效仍缺乏。来自南京医科大学的团队开展了相关
仑伐替尼目前被批准用于晚期肝癌患者的一线治疗。我们也知道PD-1抑制剂也被用于晚期肝癌患者。那仑伐替尼单药或联合PD-1抑制剂治疗中国晚期肝癌患者的真实世界疗效仍缺乏。来自南京医科大学的团队开展了相关回顾性研究,评估仑伐替尼在现实世界中对中国人群的有效性和安全性。相关结果发表在Frontiers in Oncology杂志上。
我们纳入2018年12月至2021年3月在南京大学鼓楼医院肿瘤综合中心接受Lenvatinib治疗的56例不能切除肝癌患者。有48例患者可分析且有充分的记录,其中39例肝细胞癌(HCC)患者,9例肝内胆管细胞癌(ICC)患者。共有21例HCC患者仅接受仑伐替尼治疗,而分别有18例HCC患者和9例ICC患者接受仑伐替尼联合治疗。
随访期间有20 (43.75%)例患者死亡。总体人群的mOS为22.43个月(范围为4.20-28.30个月,)。6个月、1年和18个月的OS率分别为95.74% (95% CI, 84.01-98.92)、73.08% (95% CI, 57.45-83.74)和63.22% (95% CI, 46.99-75.70)。中位PFS为8.93个月(范围:3.20-28.30个月)。

总体人群OS和PFS
接受仑伐替尼单药治疗的HCC患者的mOS和mPFS分别为22.43个月(95% CI未达到)和11.60个月(95% CI 7.46-15.74)。

HCC单药治疗OS和PFS
HCC患者仑伐替尼联合PD-1抑制剂治疗组的mOS和mPFS分别为21.77个月(95% CI, 3.68-39.86)和7.10个月(95% CI, 2.8-11.4)。

HCC联合治疗OS和PFS
然而,ICC患者仑伐替尼联合PD-1抑制剂治疗组的mOS尚未达到;而mPFS为8.63个月(95% CI, 0-17.67)。
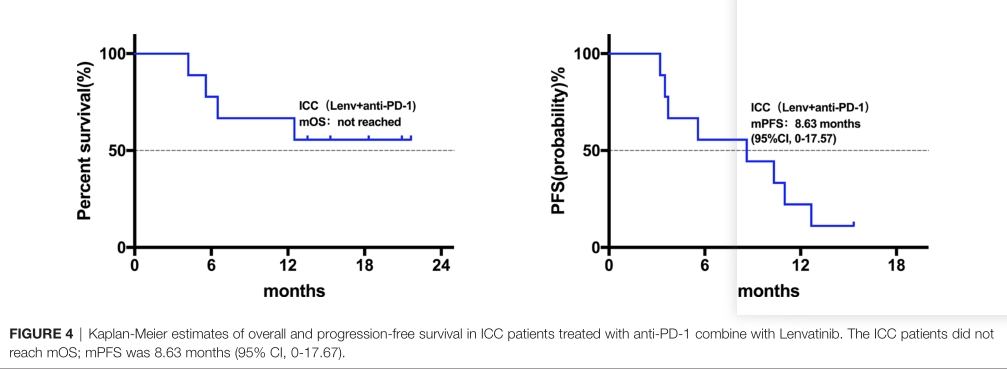
ICC单药治疗OS和PFS
21例(43.8%)和12例(25%)患者转氨酶水平升高(分别为1-2级和3-4级)。胆红素升高1 ~ 2级10例(20.8%),3 ~ 4级8例(16.7%);30例(62.5%)患者白蛋白水平为1-2级。21例(43.8%)和6例(12.5%)患者血小板下降1-2级和3-4级。19例(39.6%)和3例(6.3%)患者分别出现1-2级和3-4级碱性磷酸酶增高。此外,16例(33.3%)患者出现1-2级皮疹;没有观察到其他严重的不良事件。
一名接受联合治疗的HCC患者在第一次复查中获得完全缓解。此外,14例患者实现了部分缓解(包括2例接受仑伐替尼单药治疗的HCC患者,4例和8例接受联合治疗的ICC和HCC患者)。此外,33例患者病情稳定(其中19例单药治疗的HCC患者,5例联合治疗ICC患者,9例联合治疗HCC患者)。总ORR为31.25%;单药治疗组为9.52%。联合治疗的ICC和HCC患者分别为44.44%和50.00%。本研究疾病控制率(DCR)为100%;初次评估时时无进展性病例出现。

疗效评估
在39例HCC患者中,6例AFP基线数据为阴性。我们将剩下的33例患者分为低(≤200 ng/mL) (n=18)和高(>200 ng/mL) (n=15) AFP水平组。低AFP组3例部分缓解,15例病情稳定;高AFP组为5例PR,10例SD。基线AFP水平与影像学评估的治疗效果之间没有相关性。然而,低AFP组的OS(P = 0.0108)和PFS(P = 0.0330)均较高AFP组延长。本研究中HCC患者基线CA19-9水平与临床疗效或预后无相关性。
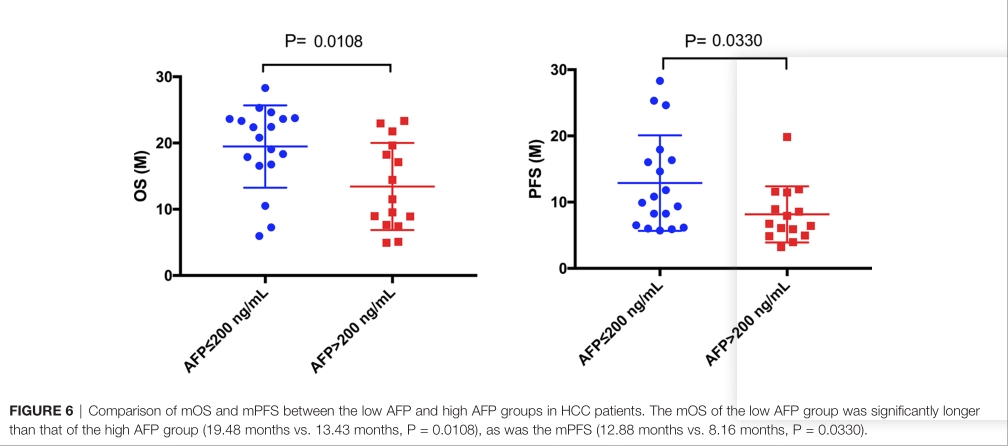
HCC患者AFP分层预后分析
此外,我们发现在9例ICC患者中,高CA-199 (>150 ng/mL)患者(n=4)与低CA-199 (≤150 ng/mL)患者(n=5)之间的OS无显著差异(P=0.1401)。但PFS差异有显著统计学意义(P=0.0230)。

ICC患者CA199分层预后分析
综上,研究表明,仑伐替尼(Lenvatinib)治疗中国晚期肝癌患者疗效显著,毒性可控。
原始出处:
Zhu S, Liu C, Dong Y, Shao J, Liu B and Shen J (2021) A Retrospective Study of Lenvatinib Monotherapy or Combined With Programmed Cell Death Protein 1 Antibody in the Treatment of Patients With Hepatocellular Carcinoma or Intrahepatic Cholangiocarcinoma in China. Front. Oncol. 11:788635. doi: 10.3389/fonc.2021.788635
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#肝癌患者#
63
#疗效和安全性#
52
学习了
79
#抑制剂#
50
#Oncol#
62
学习了
63
学习
57
#PD-1抑制剂#
65
#lenvatinib#
61
学习了
82