FDA批准放射性配体疗法Pluvicto治疗前列腺癌
2022-03-27 Allan MedSci原创
在晚期 PSMA 阳性转移性去势抵抗性前列腺癌患者的标准治疗中添加 Pluvicto 可延长基于影像学的无进展生存期和总生存期。
尽管最近前列腺癌的治疗手段取得了进展,但转移性去势抵抗性前列腺癌仍然是致命的。前列腺特异性膜抗原 (PSMA) 在转移性去势抵抗性前列腺癌中高度表达。Lutetium-177 (177Lu)–PSMA-617是一种放射性配体疗法,可向表达 PSMA 的细胞和周围的微环境提供 β 粒子辐射以杀死肿瘤细胞。
诺华制药近日宣布,FDA 已批准其 Pluvicto(Lutetium-177-PSMA-617)用于先前治疗过的 PSMA 阳性转移性去势抵抗性前列腺癌(mCRPC)成人患者。该公司表示,该决定使 Pluvicto 有望在数周内上市,该治疗将靶向化合物与治疗性放射性同位素相结合。
批准基于 III 期 VISION 试验的结果,该试验旨在评估 Pluvicto 联合标准疗法治疗 PSMA 阳性 mCRPC 患者的有效性和安全性,这些患者经先前的紫杉醇类和新型激素疗法治疗后出现疾病进展。
从 2018 年 6 月到 2019 年 10 月,共有 831 名接受了随机分组。中位随访时间为 20.9 个月。VISION 试验结果显示,与单独的标准疗法相比,接受 Pluvicto 联合标准疗法的患者死亡风险降低了 38%。与标准治疗相比,Pluvicto联合标准治疗显著延长了中位PFS(8.7 个月 vs. 3.4 个月,P<0.001)和中位OS(15.3 个月 vs. 11.3 个月,P<0.001)。Pluvicto 组 3 级或以上不良事件的发生率高于对照组(52.7% vs. 38.0%)。接受放射性配体治疗的患者中最常见的不良事件是疲劳、口干、恶心和贫血,以及食欲下降和便秘。
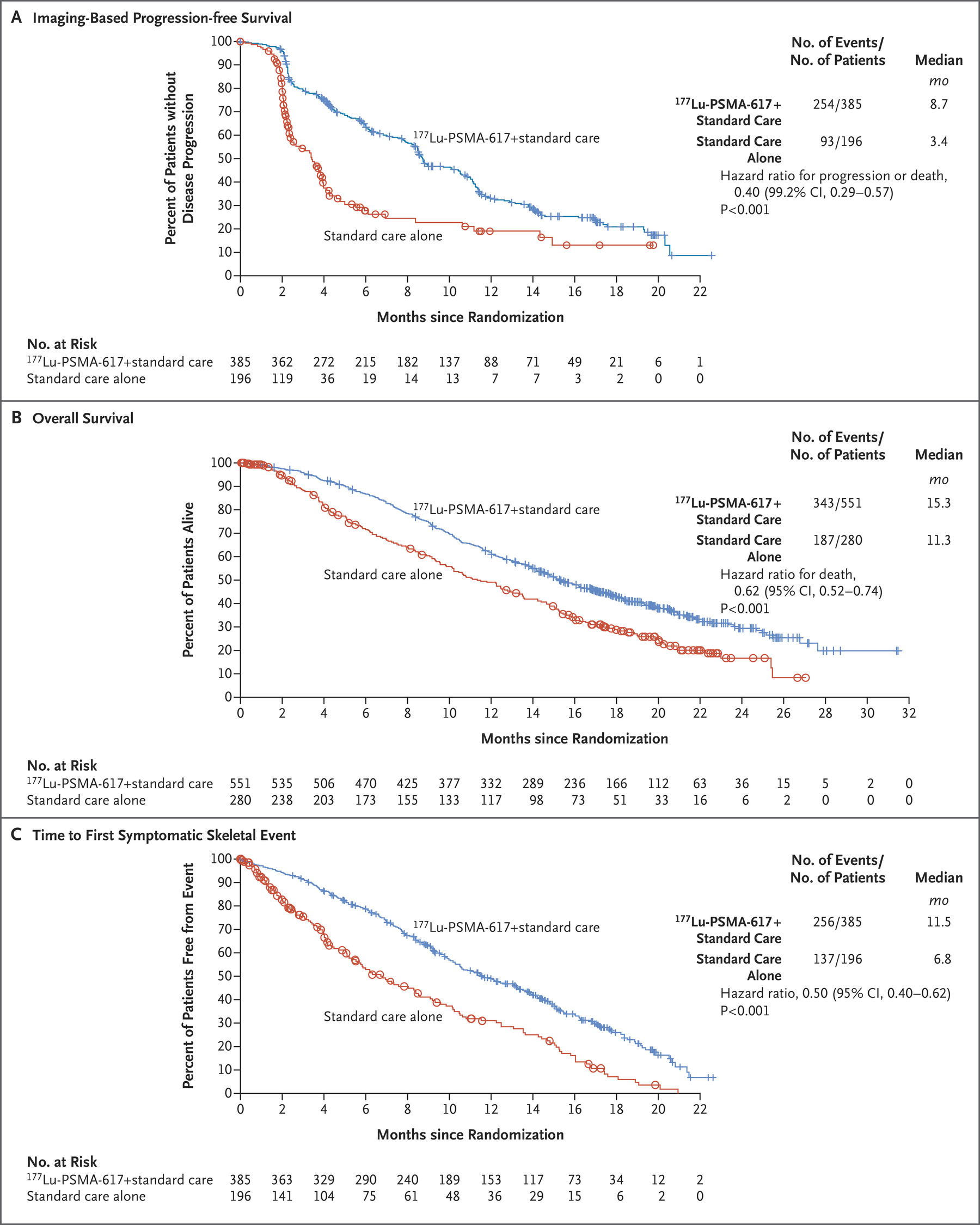
总体而言,在晚期 PSMA 阳性转移性去势抵抗性前列腺癌患者的标准治疗中添加 Pluvicto 可延长基于影像学的无进展生存期和总生存期。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
















#FDA批准#
70
#CTO#
46
不错
60
学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习
67
学习了
70
真不错
68
#学习#学习一下
71