Ardiovasc Diabetol:TyG指数与亚临床动脉粥样硬化相关性的性别差异
2021-10-18 从医路漫漫 MedSci原创
胰岛素抵抗(IR)是非糖尿病患者心血管疾病(CVD)的已知危险因素,其与高血糖或相关代谢因素有关。甘油三酯-葡萄糖(TYG)指数是通过血清葡萄糖和胰岛素浓度来定义的,认为是胰岛素抵抗的替代标记物
背景:胰岛素抵抗(IR)是非糖尿病患者心血管疾病(CVD)的已知危险因素,其与高血糖或相关代谢因素有关。甘油三酯-葡萄糖(TYG)指数是通过血清葡萄糖和胰岛素浓度来定义的,认为是胰岛素抵抗的替代标记物。
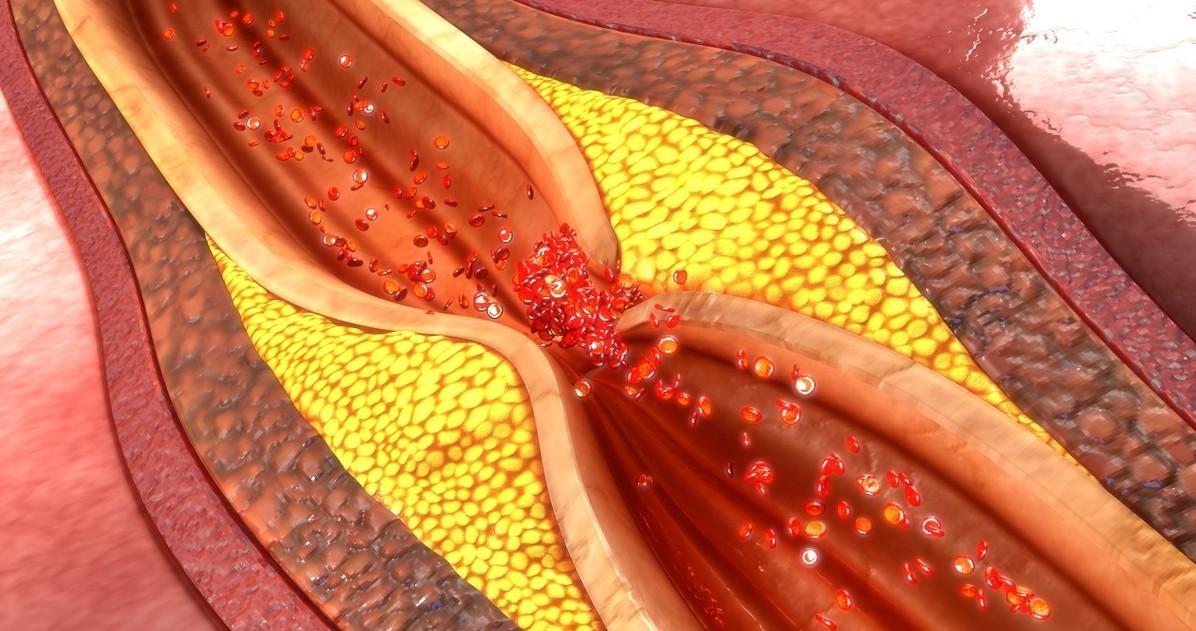
目的:本研究旨在探讨不同性别的TYG指数与亚临床动脉粥样硬化(SA)早期的关系。
方法:I-Lan纵向老龄化研究(ILAS)招募了1457名年龄在50-80岁的受试者。每名受试者均获得人口学数据和TYG指数{ln[空腹甘油三酯(mg/dL)×空腹血糖(mg/dL)]/2}。根据性别和TYG指数的第50个百分位数(≥8.55或<8.55)对患者进行进一步分层。SA定义为整个队列第75百分位数的平均颈动脉内膜-中层厚度(CIMT)。比较两组间的影像特征和SA的存在情况。用Logistic回归分析TYG指数与SA的关系。
结果:TYG指数高(≥8.55)的患者有较高的体重指数、患高血压和糖尿病的风险。与TYG指数较低的人(<8.55)相比,他们的血脂水平较高,包括总胆固醇(T-Chol)和低密度脂蛋白(LDL)。在非糖尿病女性中观察到性别差异,高TyG指数组的SA患病率明显高于低TyG指数组。在多因素Logistic回归分析中,调整传统危险因素[调整后的优势比(OR):1.510,95%CI为1.010~2.257,p=0.045]后,非糖尿病女性的高TYG指数与SA独立相关,而在非糖尿病男性中无统计学意义。TYG指数与糖尿病患者中SA的存在无关,与性别无关。
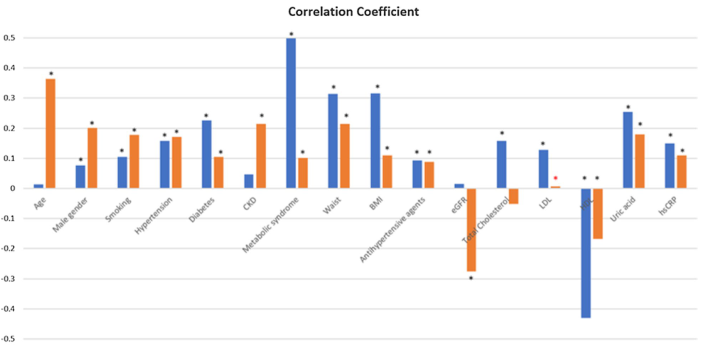
图1 TyG指数与cIMT的相关系数。黑色*表示p值< 0.001。红色*表示p值< 0.05。BMI体重指数、DM糖尿病、CKD慢性肾病、HDL高密度脂蛋白、LDL低密度脂蛋白、HbA1c血红蛋白A1c、hs-CRP高敏C反应蛋白、eGFR估计肾小球滤过率、cIMT颈动脉内膜-中膜厚度

表 非DM患者中cIMT≥0.75 mm(第75个百分点)发生率相关因素的单因素和多因素logistic回归分析(n = 1255)
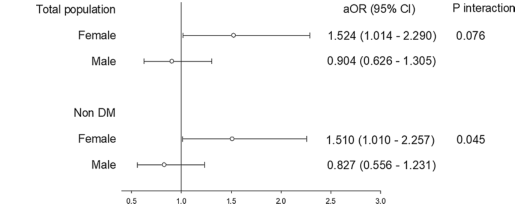
图2 全人群和非DM组的性别差异。aOR调整优势比,调整变量:年龄,BMI, HTN, CKD, UA, hsCRP
结论:在非糖尿病患者中,高TYG指数与SA和性别差异显著相关。这一结果可能突出了针对性别的风险管理策略的必要性,以预防动脉粥样硬化。
原文出处:
Lu YW, Chang CC, Chou RH,et al.Gender difference in the association between TyG index and subclinical atherosclerosis: results from the I-Lan Longitudinal Aging Study.Cardiovasc Diabetol 2021 Oct 13;20(1)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#DIA#
0
#TyG指数#
63
#BET#
47
#ASC#
48
#亚临床动脉粥样硬化#
64
#相关性#
50
#粥样硬化#
44
#动脉粥样硬化#亚临床更应关注
96