肝右叶占位之放射科病例讨论(复旦大学附属中山医院)
2015-12-10 戴亚婕 曾蒙苏 复旦大学附属中山医院放射科
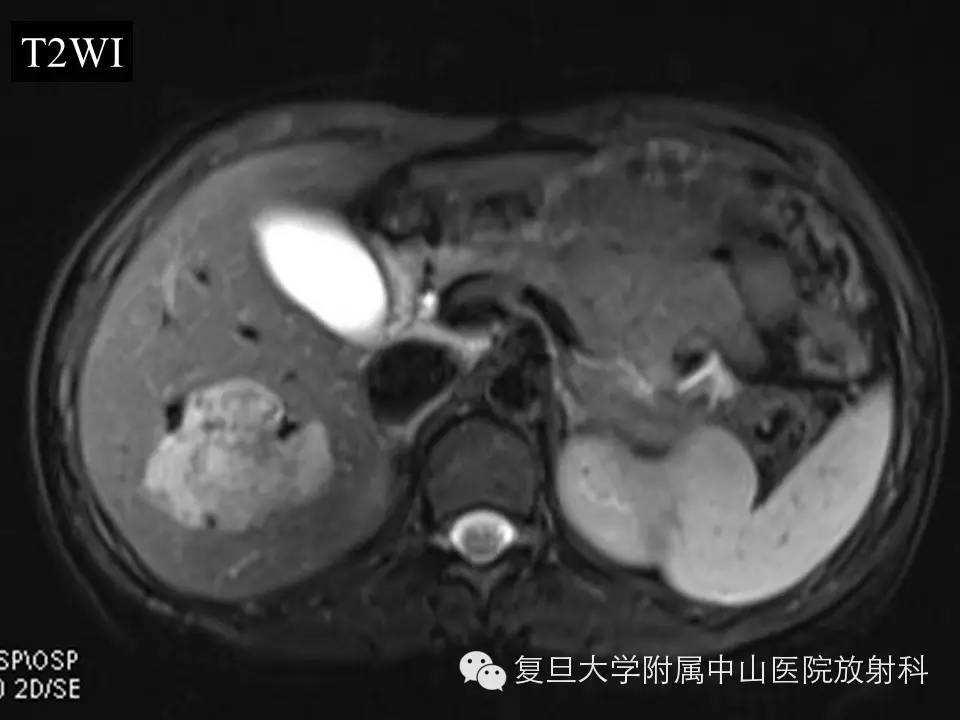
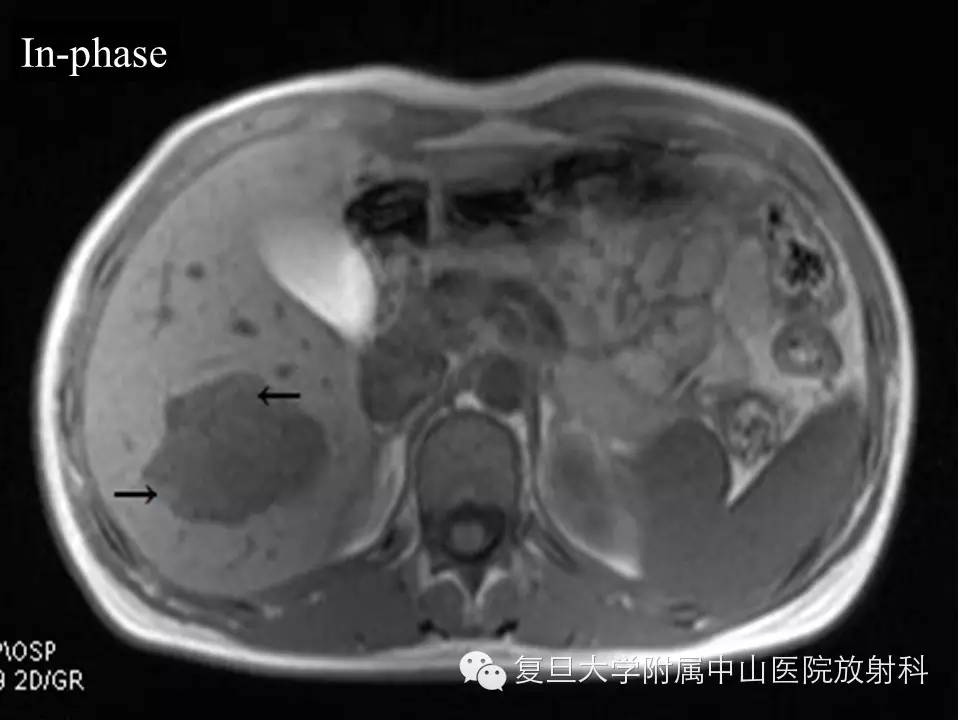
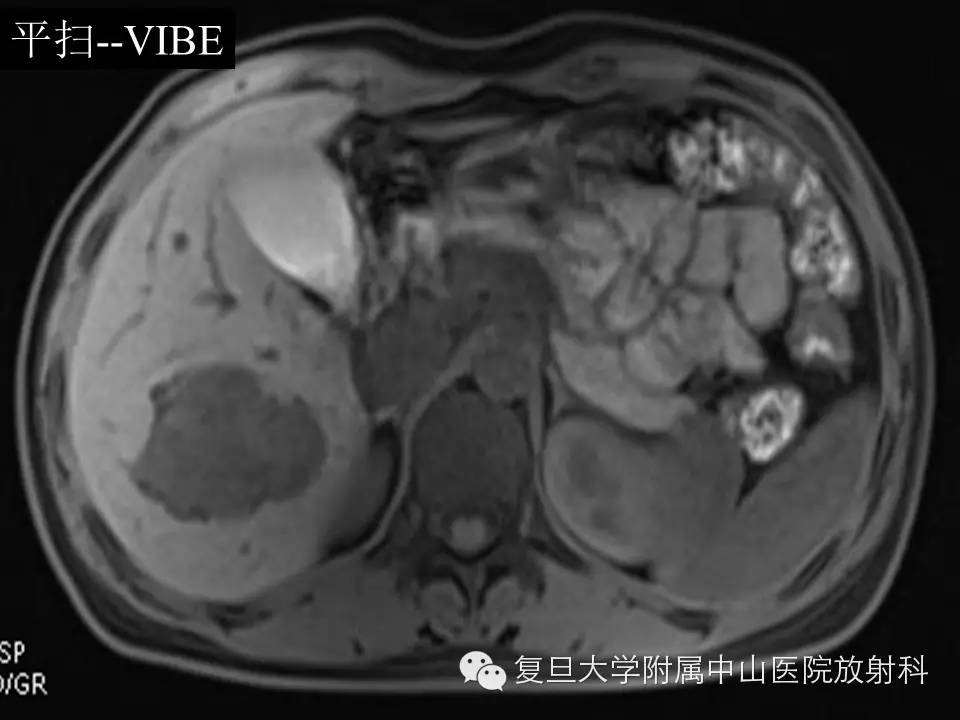
病史 女性,26岁,体检发现肝右叶占位,无不适主诉,无腹痛腹胀及皮肤黄染。外院肿瘤指标(AFP、CEA、CA19-9)均为阴性,肝功能正常,无肝炎病史,有服用紧急避孕药史。 上腹部MRI图像如下: 答案往下{nextpage} MR表现 肝右叶见团块状异常信号影,大小约4.4×6.2cm,T1WI低信号,反相位可见斑点状信号减低区(正反相位图像箭头所指)
女性,26岁,体检发现肝右叶占位,无不适主诉,无腹痛腹胀及皮肤黄染。外院肿瘤指标(AFP、CEA、CA19-9)均为阴性,肝功能正常,无肝炎病史,有服用紧急避孕药史。
上腹部MRI图像如下:


答案往下
{nextpage}
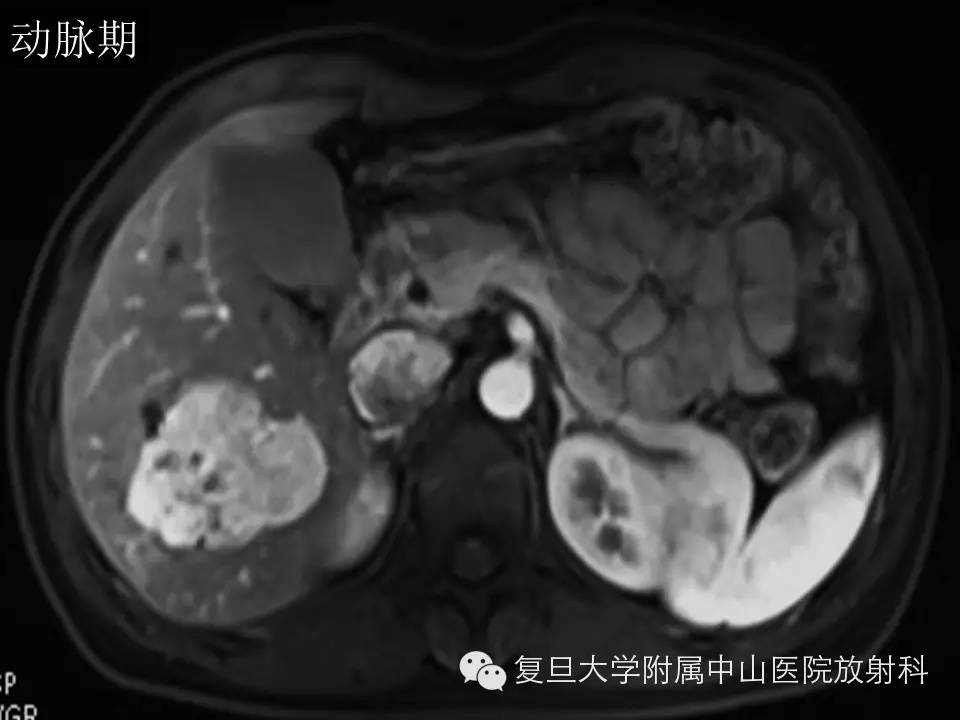
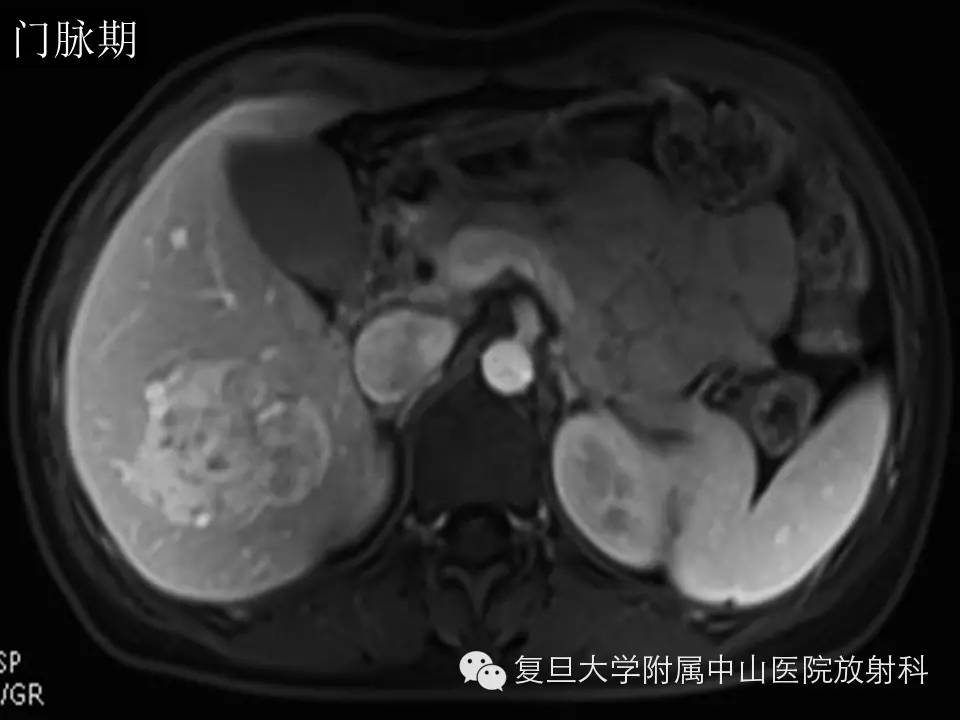
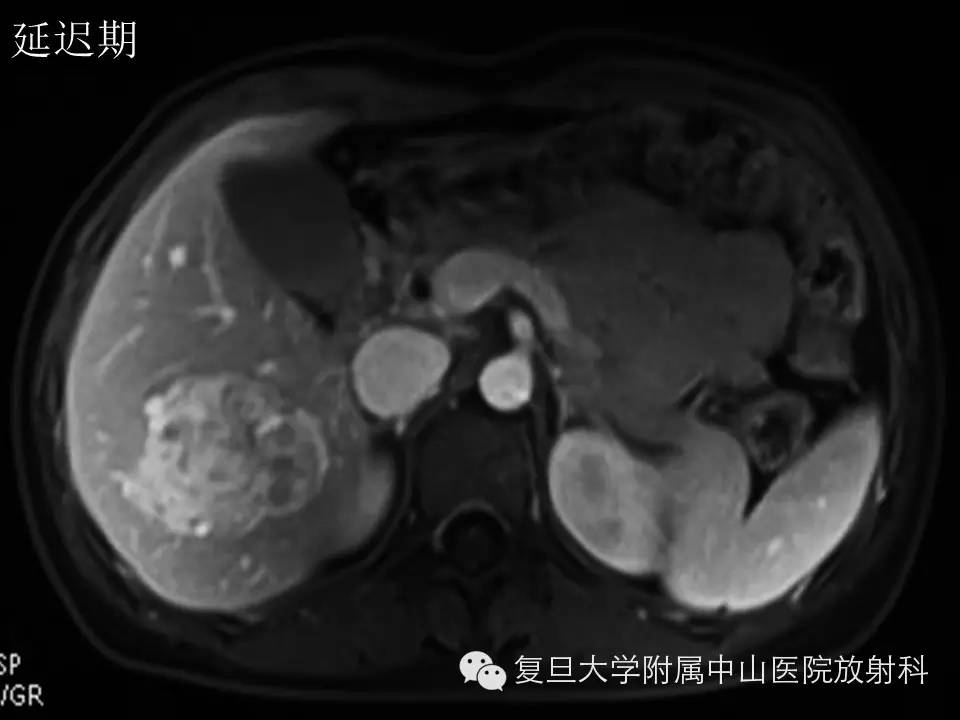
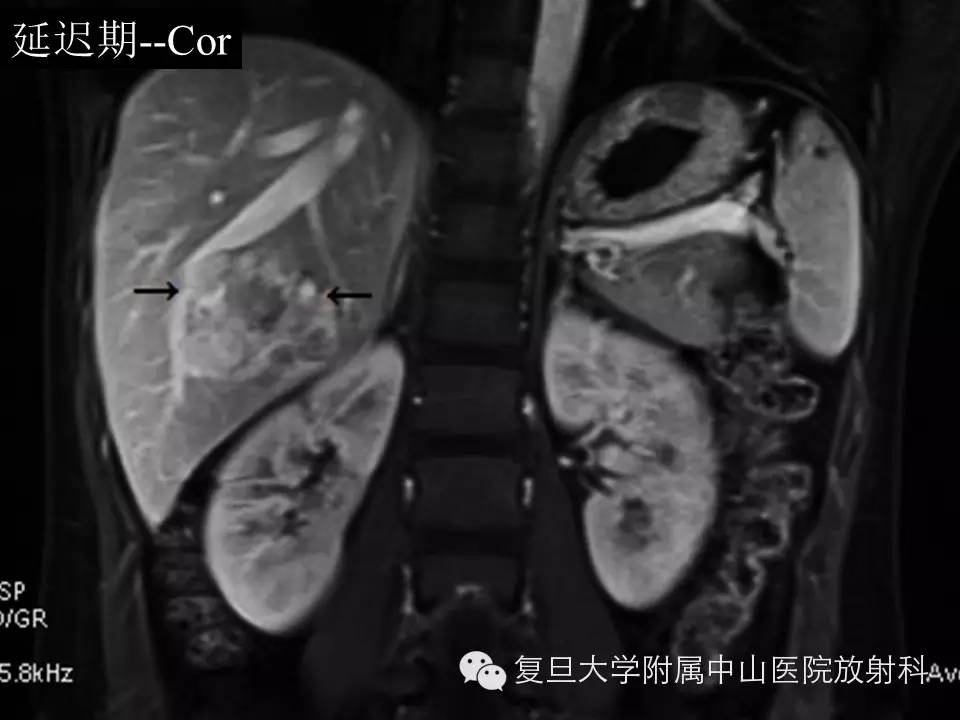
肝右叶见团块状异常信号影,大小约4.4×6.2cm,T1WI低信号,反相位可见斑点状信号减低区(正反相位图像箭头所指),T2WI及DWI呈高信号,增强后动脉期明显强化,门脉期及延迟期持续强化呈相对高密度,病灶内可见血管影(冠状位箭头)。
肝无硬化,肿瘤位于肝右叶VI段,累及部分V段及VII段,大小6.2×5.0×4.5cm。边界尚清,有包膜,无子灶,无癌栓,未见肿大淋巴结,术中出血700ml,术中输少浆血400ml,血浆400ml,术中肝门阻断两次,分别3+17min。
(肝右叶)血管平滑肌脂肪瘤,部分为上皮样血管平滑肌脂肪瘤。
讨论
肝脏血管平滑肌脂肪瘤(Hepatic angiomyolipoma,HAML)是一种罕见的良性肿瘤。肿瘤常发现于无肝硬化背景的肝脏中,多为孤立性肿块,女性好发。它由三种不同成分以不同的比例构成:平滑肌细胞,厚壁血管及成熟脂肪组织[1]。根据这三种成分的比例不同,HAML可分为混合型、脂肪瘤型(脂肪含量≥70%)、肌瘤型(脂肪含量≤10%)以及血管瘤型[2]。因此HAML的影像学表现非常多变,正确的术前诊断十分困难。
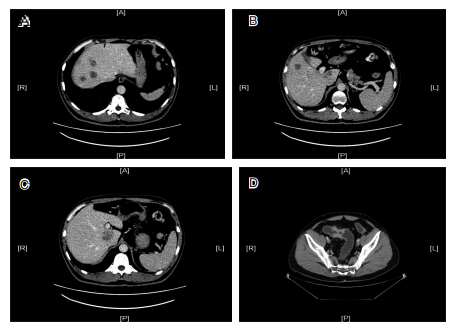
CT上,典型的HAML一般为边界清楚、不均质的低密度肿块,多为单发,没有包膜。其内可见血管平滑肌成分以及脂肪成分,部分可有钙化及囊变。增强后动脉期可见明显强化,门脉期及延迟期可见造影剂廓清或是持续强化[1] [3]。MR脂肪抑制序列有助于发现病灶内的脂肪成分,病灶内的血管在自旋回波序列中可表现为流空信号[2]。
HAML的脂肪含量可从小于10%到大于90%。肝内含脂占位需要考虑HAML,但需要与其他病变鉴别。我国为肝癌高发国家。肝细胞肝癌(HCC)合并有脂肪变时,与HAML很难鉴别。有研究[1]提出以下几点有助于鉴别HAML及HCC:1)强化程度。HAML动脉期明显强化,CT值一般超过120HU,而HCC虽动脉期明显强化,但CT值很少超过120HU。2)周围环形强化逐渐减弱。HAML周边的肿瘤血管可表现为环形强化,后期强化程度会有所减弱。而HCC典型表现——肿瘤包膜,为延迟强化。3)动脉期出现的早期引流静脉。80%HAML动脉期可见早期的引流静脉,而只有7%的HCC可见引流静脉[4]。此外肝脏含脂占位还包括较常见的有:局灶性脂肪肝、肝细胞腺瘤、局灶性结节增生、转移瘤;罕见的有:脂肪肉瘤(原发、继发)、肝脏畸胎瘤、局灶性肝脏髓外造血等,也需要考虑在内、进行鉴别
参考文献
1.Cai, P.Q., et al., Hepatic angiomyolipoma: CT and MR imaging findings with clinical-pathologic comparison. Abdom Imaging, 2013. 38(3): p. 482-9.
2.Wang, Y.J., et al., Diagnosis of hepatic angiomyolipomata using CT: report of three cases and review of the literature. Clin Radiol, 2009. 64(3): p. 329-34.
3.Ahmed, S., P.T. Johnson, and E.K. Fishman, Defining vascular signatures of benign hepatic masses: role of MDCT with 3D rendering. Abdom Imaging, 2013. 38(4): p. 755-62.
4.Jeon, T.Y., et al., Assessment of triplephase CT findings for the differentiation of fat-deficient hepatic angiomyolipoma from hepatocellular carcinoma in non-cirrhotic liver. Eur J Radiol, 2010. 73(3): p. 601-6.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#放射科#
32
#病例讨论#
37
有内容,再复习
126
………
124
#中山医院#
40
#复旦#
28