Nat Commun:伊匹木单抗和尼沃鲁米单抗治疗脑膜癌:II期研究
2021-10-13 haibei MedSci原创
最近,研究人员提出了一项单臂II期研究,18名LMD患者接受伊匹木单抗和尼沃鲁米单抗的联合治疗,直到病情进展或出现不可接受的毒性。
脑膜疾病(LMD),也被称为脑膜癌或癌变性脑膜炎,是一种以癌细胞转移性传播到脑膜为特征的现象。据报道,LMD发生在高达10%的实体瘤和5-15%的血液学恶性肿瘤中。目前,由于系统性治疗的改进,病人的生存期得到了延长,同时,随着更敏感的检测方法的发展,脑膜癌发病率正在增加。
最经常与LMD发展相关的原发性实体瘤组织学包括那些来自乳腺、肺和皮肤(黑色素瘤)的组织。虽然LMD常常与实质性疾病同时出现,但它也可以在没有实质性脑转移的情况下发生。其症状包括头痛、恶心、呕吐、神经系统功能障碍和步态不稳。不幸的是,发生LMD的病人的预后很差,平均为3至7周。
尽管LMD患者有多种治疗方式,但由于前瞻性临床试验数据的缺乏,实践中存在很大差异。多模式治疗通常是为了缓解症状和优化生活质量,而不是为了延长生存期。放射治疗方法包括立体定向放射手术(SRS),通常用于治疗整体的、体积大的和引起症状的病灶;全脑放射治疗(WBRT),用于那些身体机能较差、不可能耐受其他治疗方式的患者;以及颅脊柱照射(CSI)。
在临床试验中,全身治疗和鞘内治疗(IT)在生存获益方面的结果好坏参半,这可能是由于多种因素造成的,如原发肿瘤生物学的异质性、临床试验招募偏向于更合适的患者,以及招募人数少。

目前,这些传统治疗方法的毒副作用仍然是一个主要问题,可包括白脑病、亚急性脑病、急性小脑综合征、无菌性脑膜炎(高达43%的患者)和感染性脑膜炎(接受IT治疗中8-24%的患者)。LMD患者迫切需要能够提供有意义的生存获益和可接受的毒性的治疗方法。
最近,研究人员提出了一项单臂II期研究,18名LMD患者接受伊匹木单抗和尼沃鲁米单抗的联合治疗,直到病情进展或出现不可接受的毒性(NCT02939300)。该试验的主要终点是3个月的总生存期(OS3)。次要终点包括毒性、3个月的累积进展时间和无进展生存。西蒙的两阶段设计被用来比较18%的无效假设OS3和44%的替代假设。

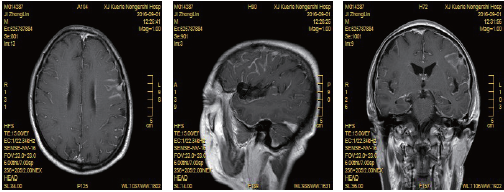
18名实体瘤LMD患者的总生存率。
根据仍然存活的患者,中位随访时间为8.0个月(范围:0.5至15.9个月)。该研究达到了主要终点,因为18名患者中有8名(OS3为0.44;90%CI:0.24至0.66)在三个月内存活。三分之一的患者经历了一次(或多次)3级或以上的不良事件。两名患者因不可接受的毒性(分别是肝炎和结肠炎)而中止了方案治疗。
最常见的不良事件包括疲劳(N = 7)、恶心(N = 6)、发烧(N = 6)、厌食(N = 6)和皮疹(N = 6)。
因此,该研究表明,联合使用伊匹木单抗和尼沃鲁米单抗具有可接受的安全性,在LMD患者中表现出有希望的活性。该结果还需要更大规模的多中心临床试验来验证。
原始出处:
Priscilla K. Brastianos al. Phase II study of ipilimumab and nivolumab in leptomeningeal carcinomatosis. Nature Communications (2021).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#脑膜癌#
63
#Nat#
45
#伊匹木单抗#
45
#COMMUN#
35