Cancer Commun:国内多中心III期研究EXELOX表明XELOX和EOX方案一线治疗晚期胃癌疗效相当
2022-03-05 yd2015 MedSci原创
研究表明,XELOX和EOX方案一线治疗晚期胃癌疗效相当。但是在分化差的腺癌和肝转移患者中,EOX较XELOX有生存获益。
在晚期胃癌(AGC)的一线治疗中,三联方案是否优于双联方案尚无共识。因此,复旦大学肿瘤医院联合国内多中心开展了III期临床研究EXELOX,目的是比较奥沙利铂加卡培他滨(XELOX)和表柔比星、奥沙利铂加卡培他滨(EOX)方案治疗AGC的疗效和安全性。相关结果发表在Cancer Communications杂志上。

EXELOX(NCT02395640)是一项开放标签、多中心、随机、前瞻性III期临床试验,在中国7个中心进行,旨在证明XELOX方案与EOX方案作为AGC患者一线治疗的非劣效性。主要终点是XELOX与EOX在意向治疗人群(ITT)的无进展生存期(PFS)的非劣效性。ITT队列包括所有随机入组的患者,无论他们是否接受了研究药物。PP队列包括符合资格标准的患者,接受至少一个周期的化疗,并进行了至少一次肿瘤反应评估。
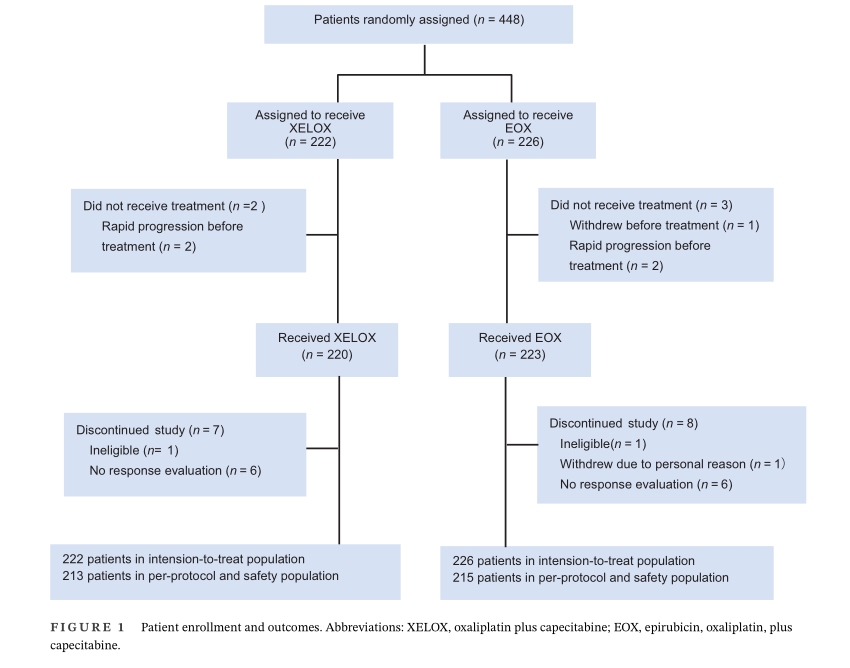
在2015年4月10日-2020年8月20日期间,448例患者被纳入,并随机分配到XELOX组(n = 222)或EOX组(n = 226)。最终,428名随机分配的患者被纳入PP组,其中213名被分配到XELOX组,215名被分配到EOX组。
对于PP组在一线治疗后出现疾病进展的患者,XELOX组有47.5%(94/198)患者接受了二线治疗,21.2%(42/198)患者无法获得二线治疗的信息。EOX组,41.3%(83/201)接受二线治疗,18.4%(37/201)失访。以紫杉醇为基础的方案最常用于二线治疗。另外,XELOX组59例患者接受最佳支持治疗,2例接受原发病灶切除,1例接受原发病灶放疗;EOX组68例患者接受最佳支持治疗,5例接受原发病灶切除术,4例接受原发病灶放疗,4例再次挑战奥沙利铂和5-氟尿嘧啶。
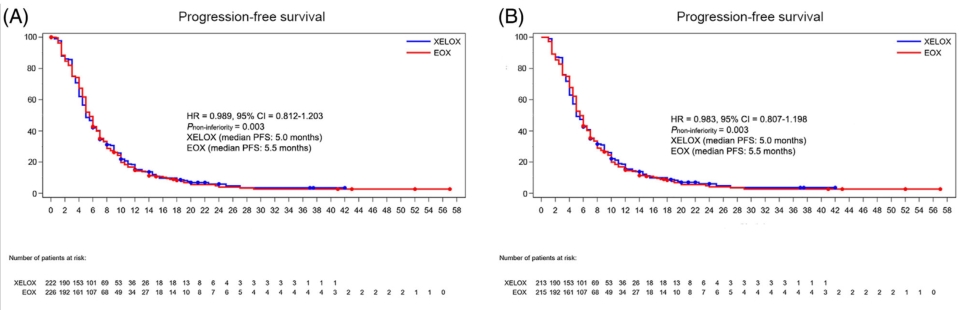
在数据截止时间(2021年2月17日),XELOX组198例(89.2%)患者和EOX组201例(88.9%)患者出现疾病进展或死亡。在ITT组中,XELOX组mPFS为5.0个月(95% CI = 4.5-6.0个月),EOX组为5.5个月(95%CI = 5.0-6.0 个月) (HR = 0.989, 95% CI = 0.812-1.203; P non-inferiority= 0.003)。 在PP队列中,XELOX组的mPFS为5.0个月 (95% CI = 5.0-6.0个月),而EOX组的mPFS为5.5 个月(95% CI = 5.0-6.0个月)(HR = 0.983, 95% CI = 0.807-1.198; P non-inferiority = 0.003)。两队列研究中两组的mPFS均达到非劣效性。
中位随访时间为13.4个月(range,3.0-59.0个月), 在 ITT队列中, 两组的mOS分别为12.0 个月(95%CI=10.4-14.0个月)和12.0个月(95% CI = 11.0-14.0个月)(HR = 1.098; 95% CI = 0.893-1.350; P = 0.384)。在PP队列中,两组的mOS 分别为12.5 个月 (95% CI = 10.5-14.0 个月)和12.0个月(95% CI = 10.0-14.0个月) (HR = 1.071; 95% CI = 0.867-1.323; P =0.529)。

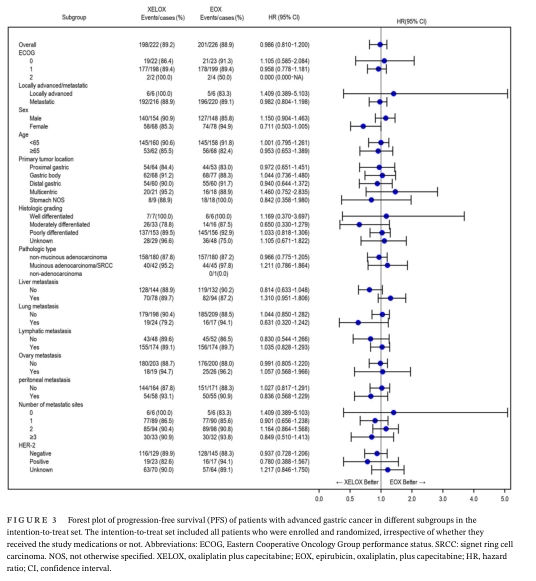
亚组分析表明,在ITT和PP组中的伴有分化差的腺癌以及肝转移患者中,EOX治疗的mOS (P = 0.021和P = 0.020)和mPFS (P = 0.073, 和P = 0.057)长于XELOX治疗。但是在其他亚组中没有显著区别。
XELOX和EOX两组的的3/4级AEs发生率分别为 42.2% (90/213)和72.5% (156/215) (P= 0.001)。EOX组的3/4级的白细胞减少,中性粒细胞减少、血小板减少,恶心、呕吐的发生率要高于XELOX组(p<0.05)。

综上,研究表明,XELOX和EOX方案一线治疗晚期胃癌疗效相当。但是在分化差的腺癌和肝转移患者中,EOX较XELOX有生存获益。
原始出处:
Zhu XD, Huang MZ, Wang YS, Feng WJ, Chen ZY, He YF, Zhang XW, Liu X, Wang CC, Zhang W, Ying JE, Wu J, Yang L, Qin YR, Luo JF, Zhao XY, Li WH, Zhang Z, Qiu LX, Geng QR, Zou JL, Zhang JY, Zheng H, Song XF, Wu SS, Zhang CY, Gong Z, Liu QQ, Wang XF, Xu Q, Wang Q, Ji JM, Zhao J, Guo WJ. XELOX doublet regimen versus EOX triplet regimen as first-line treatment for advanced gastric cancer: An open-labeled, multicenter, randomized, prospective phase III trial (EXELOX). Cancer Commun (Lond). 2022 Feb 25. doi: 10.1002/cac2.12278. Epub ahead of print. PMID: 35212487.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#III期研究#
0
#III#
45
#多中心#
45
#COMMUN#
44
#晚期胃癌#
56
#III期#
39