施一公院士再发重要成果 《PNAS》解析阿尔兹海默症关键蛋白
2016-12-09 王英 生物通
阿尔茨海默氏病(AD)是最常见的痴呆症形式,但是我们对AD的病因仍然知之甚少。最近,来自清华大学的研究人员,采用高度纯化的重组γ-分泌酶,检测了128个AD来源的早老素蛋白-1(PS1)突变对β淀粉样蛋白(Aβ42和Aβ40)产量的影响,相关研究结果发布在12月5日的《美国国家科学院院刊》(PNAS)上。领导这一研究的是清华大学的施一公(Yigong Shi)教授。施一公研究组主要致力于运用结构生

领导这一研究的是清华大学的施一公(Yigong Shi)教授。施一公研究组主要致力于运用结构生物学和生物化学的手段研究肿瘤发生和细胞凋亡的分子机制,集中于肿瘤抑制因子和细胞凋亡调节蛋白的结构和功能研究、重大疾病相关膜蛋白的结构与功能的研究、胞内生物大分子机器的结构与功能研究。回国后施一公在Nature等国际顶级期刊上发表了多篇论文,同时他也搭建起了以清华大学为中心的人才引入桥梁。2013年施一公当选为中科院院士。
2016年,施一公课题组取得了一系列研究成果,开年即在《Science》杂志发表了一项重磅成果,他们获得了分辨率为3.8埃(Å)的U4/U6.U5 三小核核糖核蛋白复合物(U4/U6.U5 tri-snRNP)三维结构,由此提供了有关剪接体(spliceosome)组装和催化的新见解。7月份又在同一期的《Science》杂志上发表两篇研究论文,采用冷冻电子显微镜(cryo-EM) 分别确定了来自酿酒酵母的催化激活剪接体(复合物Bact)的原子结构和获得了平均分辨率为3.4埃的酿酒酵母催化第一阶段剪接体(复合物C)的原子结构。。另外,在今年的2月份和3月份,施一公院士还作为通讯作者在《PNAS》上分别发表两项研究成果。
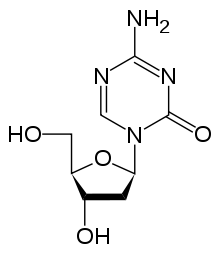
阿尔茨海默病(AD)的一个标志是,患者大脑内的β-淀粉样蛋白(Aβ)聚集成淀粉样蛋白斑块。淀粉样前体蛋白(APP)由膜内蛋白酶γ分泌酶裂解,产生了长短不一的Aβ,其中较长的肽(如β42)被认为是有害的。增加较长Aβs的比率,使其超过短的Aβs,例如,增加β42的比率超过Aβ40,可能会导致淀粉样斑块的形成和随之而来AD的发展。
AD发展的另外一个重要指标是,携带PS1、PS2或APP共同突变的患者的平均发病年龄(AAO)。一个更有害的突变可能反映在更低的AAO。对一小部分AD来源的突变的分析,支持一种强烈相关性:Aβ42/Aβ40比例越高,AAO就越低。相反,一组不同的PS1突变只显示较弱的相关性。值得注意的是,这些结论都是从有限数量的突变得出来的,缺乏统计学意义。
在这项研究中,研究人员通过将突变的PS1蛋白分别重建成包含APH-1aL的γ-分泌酶,并检测它们在体外产生Aβ42和Aβ40的能力,分析了138个报道的人类PS1突变。这些突变中大约有90%可导致Aβ42和Aβ40的产量减少。值得注意的是,这些突变的10%可导致Aβ42/Aβ40的比率下降。在由含有特定PS1突变的γ-分泌酶变体所产生的Aβ42/Aβ40比率,与患者(该突变是从他们体内分离出来的)发病时的平均年龄之间,没有统计学上显著的关联。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#重要成果#
40
#PNAS#
42
#关键蛋白#
37
#解析#
30
最近正打算做这方面,很有用
70
#阿尔兹海默#
22