JCO:内窥镜筛查干预降低食道癌死亡率
2015-05-13 MedSci MedSci原创
食道癌是世界上第八大常见癌症,估计在2012年新增456000例,也是世界上第六大致死原因,估计在2012年有400000人因食道癌而病逝。两种主要的病理亚型,食道鳞状细胞癌(ESCC)和食道腺癌占据了所有食道癌的94%。最许多经济发达的国家,过去三十五年内食道腺癌发病率出现了戏剧性地增长,尤其在白种人中;恰恰相反,ESCC的发病率出现了稳定地下降。全球范围内的食道癌负担仍旧是ESCC
食道癌是世界上第八大常见癌症,估计在2012年新增456000例,也是世界上第六大致死原因,估计在2012年有400000人因食道癌而病逝。两种主要的病理亚型,食道鳞状细胞癌(ESCC)和食道腺癌占据了所有食道癌的94%。最许多经济发达的国家,过去三十五年内食道腺癌发病率出现了戏剧性地增长,尤其在白种人中;恰恰相反,ESCC的发病率出现了稳定地下降。全球范围内的食道癌负担仍旧是ESCC,其中最严重的在亚洲,包括伊朗北部到中国东部,以及北到俄罗斯。
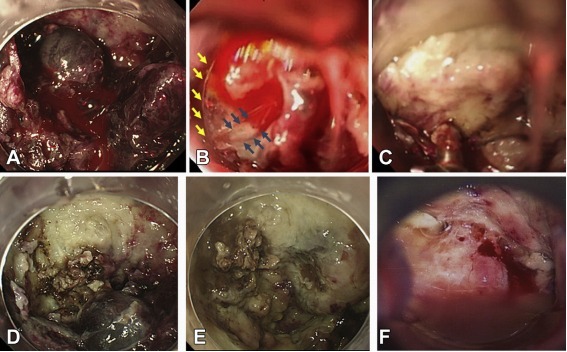
对于ESCC,目前仍然没有全球性的筛查推荐规范。自从上世纪七十年代,中国已经在此领域研究了内窥镜筛选。北京协和医学院、中国医学科学院的研究人员评估了内窥镜筛查以及干预程序是否可以降低ESCC死亡率。研究人员在ESCC高发病率社区召集了40-69岁的居民。十四个存在被选作干预社区。十个不与干预社区相毗邻的村庄作为对照组。干预组参与者曾使用卢戈碘染色内窥镜筛查,并且那些发育异常或不明原因肿瘤都经过处理。所以干预组参与者和一个包含了十分之一的对照组样本完成问卷调查。对比两组间累积的ESCC发病率和死亡率。
经过了长达十年的跟踪随访,干预组和对照组的累积死亡率是很明显的(二者分别为3.35%和5.05%)。此外,干预组有着更低的累积发病率(4.17%,对照组为5.92%)。此次研究表明内窥镜筛查和干预明显降低食道癌死亡率。肿瘤发病前的损伤的检测和治疗也导致了ESCC发病率的降低。
原始出处:
Wen-Qiang Wei et al.Long-Term Follow-Up of a Community Assignment,
One-Time Endoscopic Screening Study of Esophageal
Cancer in China.JOURNAL OF CLINICAL ONCOLOGY.Published Ahead of Print on May 4, 2015
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








嗯嗯,
136
嗯嗯,
112
对,好方法,
85
对,好方法,
103
#JCO#
36
很好的筛查方法
99
很好的资料,学习了。
72
#内窥镜#
22