Br J Ophthalmol:糖尿病视网膜病变的早期指标-视网膜动脉壁厚度
2017-07-16 吴世靖 吴婵 协和眼科资讯
糖尿病视网膜病变(DR)是一种致盲率很高的疾病,而且该类患者正在逐渐增多。为了预防糖尿病的这种微血管并发症,很多学会提出了不少预防措施,包括控制血糖、糖化血红蛋白以及血压等。一般来说,DR是一种高血糖导致的新陈代谢紊乱的病变,会增加血管基底膜成分的合成和积累,并导致基底膜的增厚。但是这些早期的变化并不能被我们常规的眼底检查发现,如果我们能在DR出现临床症状前通过直接可视化和非侵入性的手段来及早发现
糖尿病视网膜病变(DR)是一种致盲率很高的疾病,而且该类患者正在逐渐增多。为了预防糖尿病的这种微血管并发症,很多学会提出了不少预防措施,包括控制血糖、糖化血红蛋白以及血压等。一般来说,DR是一种高血糖导致的新陈代谢紊乱的病变,会增加血管基底膜成分的合成和积累,并导致基底膜的增厚。但是这些早期的变化并不能被我们常规的眼底检查发现,如果我们能在DR出现临床症状前通过直接可视化和非侵入性的手段来及早发现这些变化,我们就能尽早进行更好的干预,同时也能预防危险性很高的大血管并发症。
而该项前瞻性、观察性、横断面的临床研究通过使用高分辨率的视网膜成像方式即自适应光学扫描激光检眼镜(AOSLO),在直接可视化的情况下检测视网膜动脉壁的厚度等指标。该研究共纳入临床上不伴有DR的28名2型糖尿病患者(平均年龄53.1±9.6岁)和31名正常人(平均年龄54.5±11.0岁)。分别测量两组样本的视网膜动脉的外径、内径和视网膜动脉壁厚度(WT) (图1和图2),并收集化验室检查结果,测量颈总动脉内膜中层厚度(IMT),最后评估WT与动脉硬化危险因素的关系。
图1. 一名糖尿病患者视网膜动脉的图像
图2. 一名正常人视网膜动脉的图像
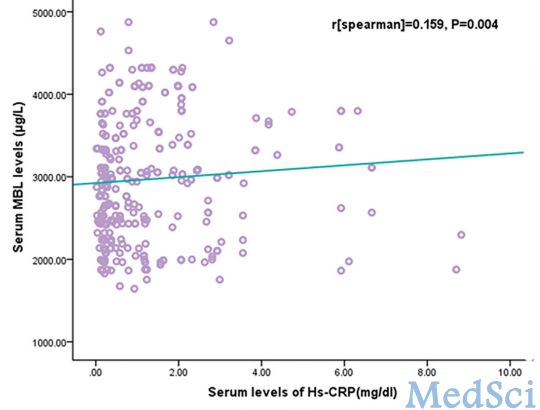
根据统计学分析结果得出,2型糖尿病患者的WT明显大于对照组,具有统计学差异(P=0.02)(表1),糖尿病患者的WT和糖化血红蛋白(HbA1c)、总胆固醇、低密度脂蛋白(LDL)和IMT具有正相关性(表2和表3)。

表2. 2型糖尿病患者视网膜动脉参数与全身系统血管参数间的关系

表3. 2型糖尿病患者视网膜动脉参数与化验室检查结果间的关系
以上结果表明,视网膜动脉壁的厚度可以作为早期发现糖尿病视网膜病变的指标,为我们能及早干预,预防严重的并发症提供一个更加有效的方法。
短评:
DR是DM的微血管并发症,也是主要的致盲性眼病之一,目前主要靠每年的散瞳检查眼底进行筛查,但在出现DR之前,可能早已出现更细微的微血管变化。高血糖引起代谢异常,可导致血管基底膜增厚,如果能够早期发现这些变化,则可以更早地进行干预并预防危险性很高的大血管并发症。
既往也有研究应用常规眼底影像来观察糖尿病患者出现DR之前的早期微血管变化,但得出的结论不一,这可能与常规眼底影像的分辨率不足有关。自适应光学技术可以校正光学波前像差,已有研究证实其可以以无创的方式提供光感受器、血流及视网膜血管壁的高分辨率图像,是普通眼底彩照无可比拟的。
本研究采用自适应光学激光共焦扫描检眼镜(Adaptive Optics Scanning Laser Ophthalmoscopy, AOSLO)的高分辨率视网膜成像模式,直接显示和评估视网膜动脉壁厚度(wall thickness, WT),文章发现,糖尿病患者视网膜动脉WT大于对照组,糖尿病患者视网膜动脉WT与HbA1c、总胆固醇、低密度脂蛋白胆固醇水平及IMT(intima-media thickness,IMT,反映大血管WT)呈正相关。这些结果表明,视网膜动脉壁测量可用于早期监测糖尿病性微血管病变。本研究也首次确定了微血管和大血管WT之间的关联,提示这种早期监测同时可以预防危险性更高的大血管并发症,有很高的临床意义。
该研究也有一些不足之处。首先,研究排除了70岁以上的患者,因为白内障会降低AOSLO的图像质量;第二,由于研究只选用清晰的图像,血糖控制不佳者可能会因为屈光间质混浊被排除,因而一些血管壁较厚眼可能未能入选。第三,本研究中的糖尿病患者患病时间较短,如果研究长期糖尿病患者,结果可能会更显着。最后,DM通常与动脉粥样硬化的其他危险因素共存,如高血压或血脂异常,因此,该研究结果需要更深入地探讨。也许在此基础上,我们可以进行更进一步的研究。未来,我们甚至可以利用计算机深度学习模式,自动判读这种早期微血管变化并给出干预提示。
原始出处:
Arichika S, Uji A, et al. Correlation of retinal arterial wall thickness with atherosclerosis predictors in type 2 diabetes without clinical retinopathy. Br J Ophthalmol. 2017 ;101(1):69-74.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言















学习了谢谢分享!
71
认真学习,不断进步,把经验分享给同好。点赞了!
68
继续学习中谢谢
70
#视网膜#
43
#视网膜病变#
36
#THA#
35
很好的想法,谢谢分享
64
学习了谢谢了。
68
学习了受益匪浅
31
学习了,谢谢
36