知临集团宣布完成针对金黄色葡萄球菌和神经母细胞瘤感染的小分子药物ALS-4和SACT-1的I期临床试验
2022-01-12 国际文传 网络
ALS-4的首次人体I期试验是一项随机、双盲、安慰剂对照、单次和多次递增剂量研究,旨在评估健康男性和女性成人志愿者口服 ALS-4 的安全性、耐受性和药物动力学。
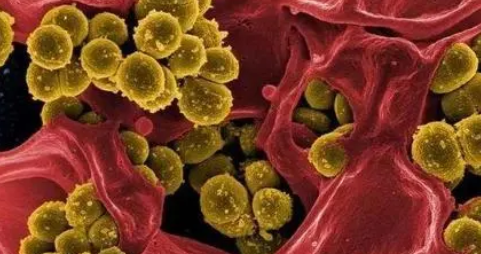
临床阶段生物制药公司知临集团有限公司(纳斯达克代码:APM,巴黎泛欧证券交易所代码:APM)(“知临集团”或“知临”)宣布已完成ALS-4(首创针对金黄色葡萄球菌引起的感染的抗毒力小分子药物,包括但不限于耐甲氧西林金黄色葡萄球菌(“MRSA”))的I期临床试验和SACT-1(一种针对神经母细胞瘤和潜在其他癌症类型的重新利用的小分子药物)的I期临床评估相对生物利用度和食物效应试验。
ALS-4的首次人体I期试验是一项随机、双盲、安慰剂对照、单次和多次递增剂量研究,旨在评估健康男性和女性成人志愿者口服 ALS-4 的安全性、耐受性和药物动力学。共72名健康受试者的单次递增剂量研究 (“SAD”) 和多次递增剂量研究 (“MAD”) 的给药和临床评估现已完成,知临欣然宣布没有受试者退出研究。当中没有观察到严重不良事件,以相关基线作相比,SAD (25-200mg)和MAD (50-100mg) 的心电图、临床实验室测试结果和身体检查以及生命体征也没有相关的临床变化。我们正等待最后一个SAD队列(300mg)和MAD队列(200mg,每天两次,持续14天)的安全性数据。凭借我们1期试验令人鼓舞的安全数据,我们有望在今年向美国FDA提交IND申请,寻求启动2期临床研究,以评估ALS-4在患者中的疗效。
SACT-1的第一个人体临床试验是在健康成年志愿者中进行的1期、随机开放、单一互换生物利用度和食物效应的研究。知临很高兴地宣布试验成功完成,在此期间未观察到严重不良事件。到目前为止,我们的试验数据令人鼓舞,我们有望在今年向美国FDA提交IND申请,以启动我们计划中的SACT-1 1b/2a期试验。
知临集团首席医疗官兼执行董事郑子俊医生评论道:“继我们之前的公告之后,我们很高兴地宣布上述ALS-4和SACT-1的临床试验已经完成。这是公司的另一个重要里程碑,也是我们在2021年制定的目标战略目标之一。这一里程碑支持知临集团于得到IND许可后开展令人兴奋的ALS-4临床II期试验和已计划的SACT-1临床Ib/2a 期试验。世界卫生组织将MRSA视为高度优先发展目标,因为它具有显著的死亡风险1 。神经母细胞瘤是一种高度未被解决的实体瘤,主要发生在小儿患者的脑外神经系统中。我们相信ALS-4和SACT-1都有可能分别有效地针对这些疾病并解决该领域未解决的需求。”
关于ALS-4
作为知临集团Acticule传染病平台的一部分,ALS-4是一种首创口服小分子药物,基于创新的针对金黄色葡萄球菌(包括MRSA)的抗毒力方法而开发。ALS-4可能透过降低选择压力来减少抗菌素抗药性,并使细菌对宿主的免疫清除高度敏感。ALS-4的目标是单独或者联合其他现有抗生素(例如万古霉素(vancomycin))使用,以实现潜在的药效。
关于SACT-1
SACT-1是一种用于治疗神经母细胞瘤的口服改用小分子药物。我们的临床前研究已经研究了SACT-1的机制,以增强肿瘤细胞死亡和抑制MYCN表达(这是通常观察到MYCN扩增的高风险或复发性神经母细胞瘤患者的常见临床诊断)。SACT-1特别被设计用于与标准护理化疗结合使用。
免责声明与前瞻性陈述
本新闻稿并不构成知临集团的任何销售要约或者购买公司证券的实质约定。
本新闻稿包含有关知临集团及其未来预期、计划和前景的陈述,这些陈述构成1995年《私人证券诉讼改革法案》界定的“前瞻性陈述”。为此目的,此处包含的任何非陈述历史事实的陈述均可被视为前瞻性陈述。在某些情况下,您可以通过诸如“可以”、“应该”、“预期”、“计划”、“预计”、“可能”、“打算”、“目标”、“预估”、“考虑”、“相信”、“估计”、“预测”、“潜在”或“继续”,或者这些术语及其他类似表达的否定形式来识别前瞻性陈述。知临集团的这些前瞻性陈述,其中包括有关申请提交和试验的预计时间表的陈述,主要基于其目前的预期及其对认为可能影响其业务、财务状况和经营业绩的未来事件和趋势的预测。这些前瞻性陈述仅反映截至本新闻稿发布之日的信息,并受若干风险、不确定性和假设的影响,包括但不限于与其宣布的管理和组织变更相关的风险、关键人员的持续服务和可用性、其通过为其他消费者细分市场提供额外产品而扩充产品线的能力、开发结果、公司预期的成长策略、业务中的预期趋势和挑战、其对供应链的期望及供应链的稳定性,以及知临集团的20-F表格、未来知临集团可能向SEC提交的其他文件,以及于2020年7月16日获得法国第20-352号法国金融市场专员的招股说明书中更加充分描述的风险。因此,这些前瞻性陈述中包含的预测可能会发生改变,实际结果可能与此处所述存在重大差异。
知临集团不承担因新信息、未来事件或其他原因而更新本新闻稿中包含的任何前瞻性陈述的义务。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言

















#母细胞瘤#
46
#I期临床#
45
#小分子#
35
#I期临床试验#
52
#金黄色葡萄球菌#
54
#细胞瘤#
55
#葡萄球菌#
60