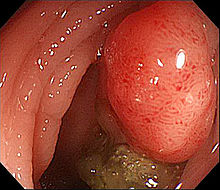
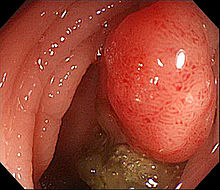
CLIN CANCER RES:结直肠癌STAT3表达与患者生存之间的关系
2017-04-08 MedSci MedSci原创
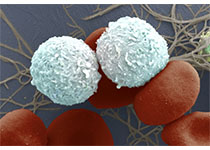
结直肠癌是消化道系统常见的恶性肿瘤,占胃肠道肿瘤的第二位。在结直肠癌患者中,高密度局部炎症浸润反应与生存期延长有关,系统性炎症增强则与不良预后有关,其中一个可能的机制就是IL6/JAK/STAT3通路。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#患者生存#
34
#STAT3#
33
#结直肠#
28
意义比较小!
45