European Radiology:LI-RADS v2018:从LR-3到LR-4,如何恰当地使用辅助特征?
2022-02-15 shaosai MedSci原创
肝脏成像报告和数据系统(LI-RADS)是一个标准化的综合分类系统,用于判析和报告肝细胞癌(HCC)风险的影像学手段。
 肝脏成像报告和数据系统(LI-RADS)是一个标准化的综合分类系统,用于判析和报告肝细胞癌(HCC)风险的影像学手段。在CT/MRI LI-RADS分类中,根据主要HCC特征的组合可以明确HCC的诊断(LR-5)。与LR-5相比,主要HCC特征的数量或组合不足的病变可被归类为LR-4或LR-3。LR-4类别表示HCC的概率很高,但没有100%的把握。事实上,相当一部分LR-4的病理结果是HCC,在这种情况下,大多数专家建议进行多学科讨论,或不进行活检就立即治疗。LR-3类别表示恶性可能性中等,意味着建议进行影像学随访而非积极治疗。鉴于这两个类别的诊治方案完全不同,进行LR-3或LR-4类别的准确鉴别在临床上十分重要。
肝脏成像报告和数据系统(LI-RADS)是一个标准化的综合分类系统,用于判析和报告肝细胞癌(HCC)风险的影像学手段。在CT/MRI LI-RADS分类中,根据主要HCC特征的组合可以明确HCC的诊断(LR-5)。与LR-5相比,主要HCC特征的数量或组合不足的病变可被归类为LR-4或LR-3。LR-4类别表示HCC的概率很高,但没有100%的把握。事实上,相当一部分LR-4的病理结果是HCC,在这种情况下,大多数专家建议进行多学科讨论,或不进行活检就立即治疗。LR-3类别表示恶性可能性中等,意味着建议进行影像学随访而非积极治疗。鉴于这两个类别的诊治方案完全不同,进行LR-3或LR-4类别的准确鉴别在临床上十分重要。
根据LI-RADS v2018,根据主要特征分类到一个类别后,可以使用辅助特征(AFs)进行进一步的分类。尽管目前的LI-RADS标准列出了各种有利于良性和恶性的AFs,但并没有提供如何应用它们进行类别调整的具体说明。
近日,发表在European Radiology杂志的一项研究在钆塞酸二钠增强MRI为背景的基础上,探讨了当肝脏结节LR-3升级为LR-4时如何适当使用AFs,为影像科医生更准确且标准的对病变进行判析提供了指导意见。
本研究回顾性地分析了在钆塞酸二钠增强MRI上被归类为LR-3/4的肝脏实性结节(≤30毫米)的MRI特征。在基于LI-RADS诊断表的LR-3观察中,进行了逻辑回归分析,以确定提示肝细胞癌(HCC)而不是非恶性结节的AFs。使用McNemar检验,根据AF在类别调整中的应用原则,比较了最终LR-4类别对HCC诊断的敏感度和特异度。
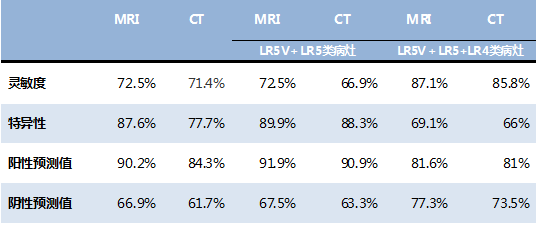
共评估了252名患者的336个肝脏结节(191个HCC;145个非恶性)。根据主要的HCC特征,248个结节(123个HCC)被分配为基于分类标准的LR-3,88个结节(68个HCC)被分配为基标准格的LR-4。在基于标准格的LR-3观察中,相对于非恶性结节而言,轻度-中度T2高信号被确定为HCC的独立预测因素(几率=3.01,p=0.002)。对于HCC的诊断,最终LR-4的不同标准:仅基于标准的-LR-4,允许仅使用T2高信号的类别升级,或使用有利于恶性的任何AF,其敏感性分别为35.6%(68/191)、53.9%(103/191)和88.5%(169/191),特异性为86.2%(125/145)、75.9%(110/145)和21.4%(31/145),彼此之间存在统计学差异(所有P<0.001)。
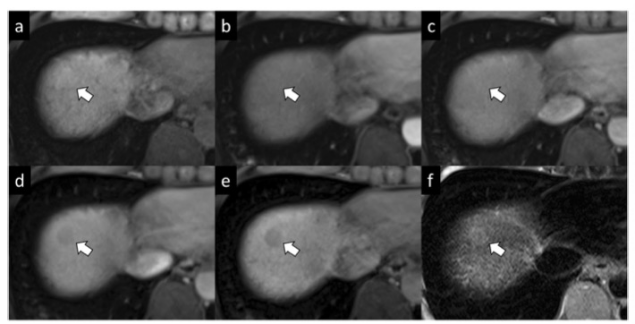
图 一名56岁的乙肝病毒相关肝硬化患者,组织学证明为肝细胞癌(HCC)。3.0T增强MRI的轴位图像(a-f)显示肝脏第八段有一个1.8厘米的结节(箭头),在(a)对比前T1加权MRI和(b)动脉相以及(c)门静脉相(PVP)上显示为等密度。在(c)PVP或(d)平衡期(TP)图像上均未见增强。根据主要的HCC特征,这个结节将被定为LR-3(恶性肿瘤的中等可能性)。然而,根据有利于恶性的辅助特征。(d)TP低密度,(e)肝胆相低密度,和(f)轴向T2加权图像上的轻度高信号,它可以升级为LR-4(可能是HCC)。
本研究表明,虽然在LI-RADS类别调整中应用MRI AFs可以提高LR-4类别对HCC诊断的敏感性,但可能伴随着特异性的降低。只应用轻度-中度T2高信号这一表现,即HCC而不是非恶性结节的重要AF,似乎更适合于将LR-3升级为LR-4这种情况。这些结果与目前LI-RADS推荐的 "可选择 "使用AFs一致,而且有助于为将LR-3升级到LR-4类别提供更具体的指导。
原文出处:
Sun Kyung Jeon,Ijin Joo,Jae Seok Bae,et al.LI-RADS v2018: how to appropriately use ancillary features in category adjustment from intermediate probability of malignancy (LR-3) to probably HCC (LR-4) on gadoxetic acid-enhanced MRI.DOI:10.1007/s00330-021-08116-0
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#ADS#
0
#LI-RADS#
61
#PE#
32
#RADS#
62