Cell Stem Cell:造血干细胞直接响应感染,既“杀敌”也“自损”
2017-07-24 佚名 生物探索
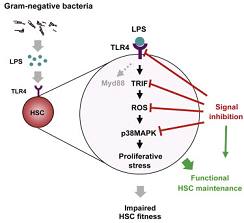
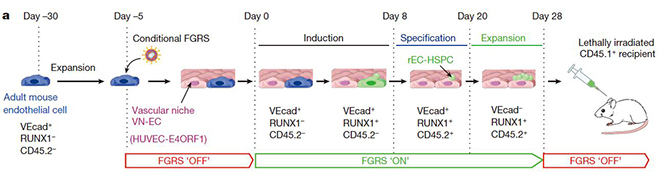
造血干细胞是血液系统中的成体干细胞,具有自我更新、多向分化的潜能。造血干细胞可以分化形成各类成熟血细胞,以此满足生理需求和调节各细胞组分之间的平衡。如果发生严重感染,造血干细胞会生成更多的白细胞以抵抗病原物。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#stem cell#
35
#Cell#
23
#CEL#
35
#造血干细胞#
30
#STEM#
24
#造血#
28
学习了新知识
47
学习,谢谢分享
48