Arthritis Rheumatol:特立帕肽对类风湿性关节炎患者关节侵蚀的疗效如何?
2017-05-29 xing.T MedSci原创
由此可见,采用特立帕肽治疗一年并没有显著减少采用TNFi治疗控制疾病活动的RA患者手部或手腕的侵蚀体积。
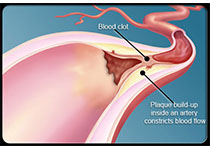
关节的侵蚀与类风湿关节炎(RA)患者的残疾相关。RA的生物治疗可以减缓关节侵蚀的进展,但关节侵蚀很少发生愈合。近日,风湿疾病领域权威杂志Arthritis & Rheumatology上发表了一篇研究文章,研究人员旨在评估合成代谢剂特立帕肽对采用肿瘤坏死因子拮抗剂(TNFi)治疗的RA患者关节侵蚀体积的影响。
研究人员对24例采用TNFi控制疾病活动至少三个月的侵蚀性RA、骨质疏松患者进行了一项随机对照试验。一半参与者被随机分配接受特立帕肽治疗一年,其他人组成对照组。研究人员并未对受试者和主要的风湿病专家治疗分组采取盲法,但所有的结果评估是在分组不知情的情况下进行的。该研究的主要结局为六个解剖位点经计算机断层扫描测得的侵蚀体积变化情况。在每一只手和解剖部位的显著性是基于双尾检验,p值 < 0.05被认为具有统计学意义。
研究人员发现治疗组间的基线特征平衡良好。在治疗52周后,采用特立帕肽治疗组侵蚀体积的变化中位数(四分位数)为-0.4立方毫米(-34.5至29.6),并与对照组的9.1立方毫米没有显著差异(-29.6至26.4)(P=0.28)。在桡骨、尺骨或掌指关节处的侵蚀体积无显著变化。特立帕肽治疗组患者股骨颈和腰椎的骨密度显著改善。
由此可见,采用特立帕肽治疗一年并没有显著减少采用TNFi治疗控制疾病活动的RA患者手部或手腕的侵蚀体积。
原始出处:
D.H. Solomon, et al. Effects of Teriparatide on Joint Erosions in Rheumatoid Arthritis: A Randomized Controlled Trial. Arthritis & Rheumatology.2017. http://onlinelibrary.wiley.com/doi/10.1002/art.40156/full
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Arthritis#
41
学习了?新知识。
57
#关节炎#
36
#类风湿#
32
#ART#
37
#风湿性关节炎#
32
#特立帕肽#
0
好好努力学习
48
学习了,感谢分享。
47