Eur J Cancer:瑞格菲尼/索拉非尼抑制脑膜瘤细胞的生长与侵袭
2017-12-31 MedSci MedSci原创
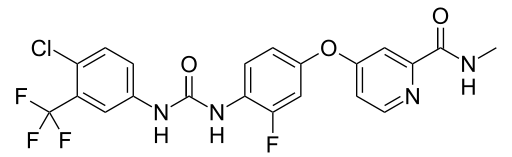
对于不可切除和/或侵袭性脑膜瘤的全身化疗结果,目前仍然不令人满意。PDGF受体(PDGFR)介导的有丝分裂信号传导在脑膜瘤中已被证明处于激活状态。因此,研究者们评估了临床上表征良好的受体酪氨酸激酶抑制剂瑞格菲尼/索拉非尼是否具有PDGFR的抑制作用,研究者们使用IOMM-Lee脑膜瘤细胞模型,通过磁共振成像监测,评估了瑞格菲尼/索拉非尼的细胞毒性作用,抑制增殖作用,诱导细胞凋亡以及抑制细胞侵袭的作
对于不可切除和/或侵袭性脑膜瘤的全身化疗结果,目前仍然不令人满意。PDGF受体(PDGFR)介导的有丝分裂信号传导在脑膜瘤中已被证明处于激活状态。因此,研究者们评估了临床上表征良好患者,观察受体酪氨酸激酶抑制剂瑞格菲尼/索拉非尼是否具有抑制作用,研究者们使用IOMM-Lee脑膜瘤细胞模型,通过磁共振成像监测,评估了瑞格菲尼/索拉非尼的细胞毒性作用,抑制增殖作用,诱导细胞凋亡以及抑制细胞侵袭的作用。
结果显示,瑞格菲尼/索拉非尼对恶性IOMM-Lee细胞的存活具有显著抑制作用,且能够诱导肿瘤细胞凋亡。Western Blot 结果表明这两种药物主要通过抑制ERK(p44 / 42)的磷酸化,进而下调PDGFR的表达。两种药物还显示出了对肿瘤细胞运动性和侵袭性的显著抑制。在体实验中,具有原位脑膜瘤异种移植物的小鼠在瑞格菲尼/索拉非尼治疗后肿瘤体积显著缩小。对体内生长的肿瘤细胞的分析再次证明了这两种药物导致了PDGFR表达水平的显著降低。
因此瑞格菲尼/索拉非尼主要通过靶向PDGFR和ERK信号通路来实现抗脑膜瘤细胞的生长与侵袭的目的。
不过,梅斯医学需要提醒的是,这仅仅是细胞学水平的研究,在人体的作用还是未知的。
原始出处:
Tuchen, Marcus, et al. "Receptor tyrosine kinase inhibition by regorafenib/sorafenib inhibits growth and invasion of meningioma cells." European Journal of Cancer 2017 73: 9-21. doi.org/10.1016/j.ejca.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#脑膜瘤#
38
谢谢分享学习了
63
不错的文章值得推荐
51
谢谢分享学习了
63