JCO: BRAF V600E在小儿轻度胶质瘤中的治疗和预后意义
2017-07-23 Yara MedSci原创
在大多数BRAF V600E PLGG患者中,都有进行性疾病发生并且对常规化学疗法缺乏反应。
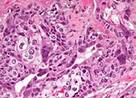
BRAF V600E是在小儿轻度胶质瘤(PLGG)的人群中检测到的有较高频率的潜在突变。但是该突变在不同肿瘤中的生物学和临床效果仍然未知。
研究人员对长期随访的510名PLGG患者进行了临床和遗传背景研究;并将99名BRAF V600E突变的PLGG患者的临床和治疗数据与另一包括BRAF V600E突变型PLGG(n = 180)患者的大型国际独立队列数据进行比较。
研究发现:在405名PLGG患者中,有69名在多个组织和部位,包括中线位置检测到BRAF V600E突变(17%)。在化疗和放射治疗后,BRAF V600E PLGG患者往往表现不佳,而且其10年无进展生存率为27%,而BRAF 野生型PLGG患者组10年无进展生存率为60.2%。其他的临床和分子实验结果显示,肿瘤切除程度和CDKN2A缺失都会独立贡献于BRAF V600E PLGG患者的不良治疗效果。在独立队列中观察到CDKN2A和肿瘤切除具有相似的独立作用。此外,成像定量分析显示:在大多数BRAF V600E PLGG患者中,都有进行性疾病发生并且对常规化学疗法缺乏反应。
原文出处:
Alvaro Lassaletta, et al. Therapeutic and Prognostic Implications of BRAF V600E in Pediatric Low-Grade Gliomas. Journal of Clinical Oncology ,July 20, 2017
本文为梅斯医生(Medsci)原创整理编译,转载需授权!
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#JCO#
34
#BRAF#
32
#预后意义#
30