EClinicalMedicine:一项3期随机、双盲研究表明:MIL60或可作为晚期或复发性非鳞状非小细胞肺癌的替代疗法
2022-05-28 “无癌界”公众号 “无癌界”公众号
减少肿瘤的血管形成,从而抑制肿瘤的生长。2015年,贝伐珠单抗联合铂双重化疗被批准为中国晚期或复发性非鳞状非小细胞肺癌的一线治疗药物。但是由于各种因素,如报销不足和高成本,患者能够使用贝伐珠单抗治疗的
导语
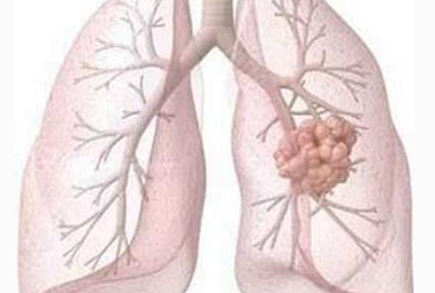
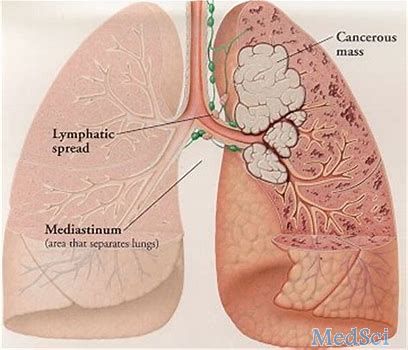
肺癌是全球癌症相关死亡的主要原因,非小细胞肺癌(NSCLC)占所有肺癌病例的85%。血管内皮生长因子(VEGF)是正常和恶性肿瘤血管生成的主要调节因子。研究发现包括NSCLC在内的大多数人类肿瘤组织中VEGF表达明显增加,在许多情况下,VEGF与复发、转移和死亡风险增加有关。
贝伐珠单抗是一种重组人源化单克隆抗体,可以选择性地与VEGF结合并阻断其生物活性,减少肿瘤的血管形成,从而抑制肿瘤的生长。2015年,贝伐珠单抗联合铂双重化疗被批准为中国晚期或复发性非鳞状非小细胞肺癌的一线治疗药物。但是由于各种因素,如报销不足和高成本,患者能够使用贝伐珠单抗治疗的机会有限。
2021年11月19日,一项名为“Efficacy and safety of MIL60 compared with bevacizumab in advanced or recurrent non-squamous non-small cell lung cancer: a phase 3 randomized, double-blind study”的研究论文发布于《柳叶刀》子刊EClinicalMedicine,本研究由中国医学科学院北京协和医学院国家肿瘤中心/国家肿瘤临床研究中心/肿瘤医院王杰教授牵头,旨在评估贝伐珠单抗生物仿制药MIL60在中国晚期或复发性非鳞状NSCLC患者中的有效性和安全性的等效性,结果表明MIL60或可作为晚期或复发性非鳞状非小细胞肺癌的替代疗法。
01
方法
将未经治疗的晚期或复发性NSCLC患者随机(1:1)接受MIL60或贝伐单抗联合紫杉醇/卡铂治疗。非进展性疾病患者继续维持单剂MIL60,直到疾病进展,或出现无法耐受的毒性。主要终点是独立审查委员会(IRC)使用RECIST 1.1计算的12周客观有效率(ORR12)。如果ORR比位于0.75和1/0.75之间,则建立生物等效性。该试验已在clinicaltrials注册,gov(NCT03196986)。
02 结果
1、基线特征
2017年8月23日至2019年5月8日期间,筛查了764名患者,517名患者被随机分配到MIL60组(n=257)和贝伐单抗组(n=260) 。其中FAS人群包括MIL60组的253名患者和贝伐单抗组的255名患者。515名患者被纳入安全性分析集(SS),MIL60组和贝伐单抗组分别有256名和259名患者。结果说明各组之间的基线特征平衡良好(表格1)。
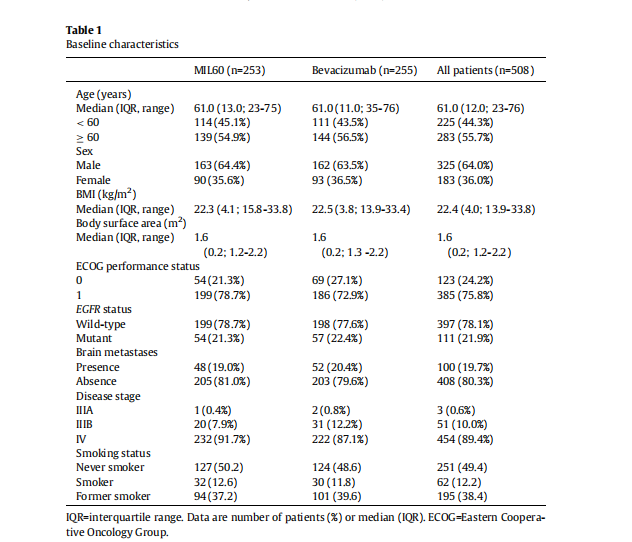
来源:EClinicalMedicine
2、功效
在FAS中,IRC评估的ORR12为48.6%(95%CI 42.6-57.8),而MIL60组和贝伐单抗组分别为43.1%(37.4-52.1)(表2)。对于ORR12,MIL60与贝伐单抗的风险比为1.14(90%可信区间0.97-1.33),在方案规定的等效边界值范围内(0.75,1/0.75)。
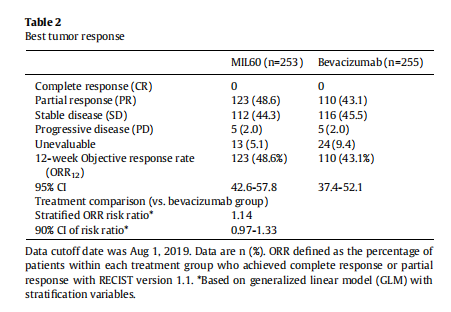
来源:EClinicalMedicine
另外MIL60的中位DOR为5.7个月(95%Cl 4.5-6.2),贝伐珠单抗为5.6个月(95%Cl 4.3-6.4)。在中位数PFS中没有显着差异(7.2 vs. 8.1个月;HR1.01,95%Cl 0.78~1.30,p=0.9606)和OS(19.3 vs. 16.3个月);HR 0.81,95%Cl 0.64~1.02,p=0.0755)。
3、安全性
MIL60组的180名(70.3%)患者和贝伐珠单抗组的188名(72.6%)患者发生了3级或更高的TEAE。两组中最常见的3级治疗相关TEAEs是中性粒细胞减少症,细胞减少症,高血压,骨髓抑制和发热性中性粒细胞减少症(表3)。

来源:EClinicalMedicine
结果说明了MIL60组和贝伐珠单抗组安全性相似,且试验共对515例患者进行了ADA分析,发现治疗期间未发现阳性结果。
4、群体药代动力学分析
在单一和稳定状态下,与贝伐单抗组相比,MIL60组上述暴露几何平均比(AUC和Cmax)的90%Cl在80%-125%之间。
在NSCLC患者中,MIL60和贝伐单抗的Cl或V2没有显着差异。PK参数还表明,晚期或复发性NSCLC患者中,MIL60和贝伐单抗的暴露量没有显着差异。
总之,该研究为MIL60在疗效、安全性、免疫原性等方面的临床等效性提供了强有力的证据,为晚期或复发性非鳞状非小细胞肺癌患者提供了一种具有成本效益的替代疗法。
原始出处:
Rui Wan , Xiaorong Dong ,Qun Chen ,Yan Yu ,Shujun Yang ,Xiaochun Zhang,jie wang ,et al.Efficacy and safety of MIL60 compared with bevacizumab in advanced or recurrent non-squamous non-small cell lung cancer: a phase 3 randomized, double-blind study.eClinicalMedicine, Vol 42, 101187.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#DIC#
0
#复发性#
81
#替代疗法#
0
#IL6#
50
#非小细胞#
69
#CIN#
31
#非鳞状非小细胞肺癌#
49
#clinical#
35
#双盲#
39
#Medicine#
34