陈成伟:CHB初治药物选择 [APASL 2012]
2012-03-10 MedSci 中国医学论坛报
慢性乙型肝炎(CHB)患者初治药物的选择是治疗成功的关键。新修订的APASL慢性乙型肝炎诊疗指南(简称2012年版指南)于2012年2月16-19日在台北召开的22届APASL年会上颁布。新版指南在强调长期治疗重要性的同时,指出初治药物选择原则应为强效低耐药,并将恩替卡韦(ETV)和替诺福韦(TDF)列为优先选用(ⅠA)。此也为本次指南更新最值得关注的亮点。 下面由中华医学会肝病学
慢性乙型肝炎(CHB)患者初治药物的选择是治疗成功的关键。新修订的APASL慢性乙型肝炎诊疗指南(简称2012年版指南)于2012年2月16-19日在台北召开的22届APASL年会上颁布。新版指南在强调长期治疗重要性的同时,指出初治药物选择原则应为强效低耐药,并将恩替卡韦(ETV)和替诺福韦(TDF)列为优先选用(ⅠA)。此也为本次指南更新最值得关注的亮点。
下面由中华医学会肝病学分会副主任委员、上海南京军区临床肝病中心陈成伟教授结合更新版指南对CHB初始抗病毒治疗策略进行解读。
CHB治疗是长期过程
新版指南继续充分肯定和强调了长期治疗管理的重要性,强调持久抑制乙肝病毒(HBV)复制是抗病毒治疗的首要目标。近期治疗目标为达到“初步应答”,即乙肝e抗原(HBeAg)的血清学转换和(或)HBV DNA抑制,丙氨酸氨基转移酶(ALT)水平恢复正常,预防肝脏失代偿,达到“持久应答”,即降低治疗期间/治疗后肝脏坏死性炎症和肝纤维化的发生。最终长期治疗目标是预防肝脏失代偿、减少或预防进展到肝硬化和(或)肝癌,并延长生存期。
HBV共价闭合环状DNA(cccDNA)半衰期长,且现有的抗病毒药物仅能有效抑制外周血中的HBV DNA,对细胞核内cccDNA的影响甚微,因此其存在是HBV持续感染而难以根治的重要原因,使大多数患者接受抗病毒治疗后并不能彻底清除病毒。有研究显示,即使治疗后乙肝表面抗原(HBsAg)消失,仍有79%患者的肝内可检出cccDNA。因此,为了完全清除病毒,必须进行长期治疗。
HBV持续感染可通过炎症反应导致肝纤维化甚至肝硬化的发生。肝纤维化是一个缓慢进展的过程,如在此期间能予足够长时间的抗病毒治疗,有效去除导致纤维化的因素,肝纤维化甚至是肝硬化都有可能有所消退,并可减少肝癌发生风险。从这一角度看,CHB的治疗也应是一个长期过程。
抗病毒治疗适应证
新版指南强调了在抗病毒治疗用药前应对患者进行全面评估和提供咨询的必要性,除进展期的肝纤维化或肝硬化的患者外,HBV复制但ALT水平持续正常或轻度增高的患者不必治疗,但需要充分追踪随访,并每3~6月监测肝癌标志物(ⅠA)。
除有肝硬化临床证据的患者外,ALT水平较高或缓慢升高的患者及年龄超过40岁的患者均应进行肝纤维化评估(ⅡA)。
新版指南对抗病毒治疗适应证未作更改,即为ALT≥2倍正常上限(ULN)、HBV DNA>2.0×104 IU/ml、HBeAg阳性的CHB患者;或ALT≥2倍ULN、HBV DNA>2.0×103 IU/ml、HBeAg阴性的CHB患者。若有进展期肝纤维化或肝硬化,不论ALT是否升高,均应考虑开始抗病毒治疗(ⅠA)。一旦有肝功能失代偿倾向或明显肝功能失代偿的肝炎患者,应尽早治疗(ⅡA )。
初治药物选择原则:尽量选择强效低耐药药物
初治药物选择原则
初始药物选择应综合考虑药物疗效、安全性、耐药风险、患者依从性及费用可承受性。
首先,强效的抗病毒药物可早期达到病毒载量不可测,且抗病毒能力随时间延长日益明显。
其次,耐药风险是影响CHB长期治疗目标的重要因素,耐药不但会导致疾病进展,也会明显增加患者经济负担,因此初治药物选择对预防耐药发生也至关重要。良好的安全性和耐受性是CHB患者坚持长期治疗的前提,且影响长期依从性的很多因素也与药物选择有关。因此,初治治疗药物的选择在长期管理和总体目标的实现中占据主要地位。
初始推荐ETV为一线用药
目前所有国内外指南均未推荐对CHB患者初治进行联合治疗。
新版指南建议,初治患者可以用普通干扰素5~10 MU每周3次(ⅠB)或聚乙二醇干扰素α-2a 180 μg、每周1次,或聚乙二醇干扰素α-2b 1~1.5μg/kg、每周1次(ⅠA),也可用ETV 0.5 mg/d(ⅠA),TDF 300 mg/d(ⅠA),ADV 10 mg/d(ⅠB),LdT600 mg/d(ⅠB),或LAM 100 mg/d(ⅠB)。指南对推荐等级给出了明确建议,ETV和TDF被优先推荐(ⅠA),充分体现了亚太专家对初治药物选择的观点更新,强效低耐药是初治药物选择的原则。在优先推荐药物不适用、不可获得等特殊情况下,LdT、ADV和LAM等药物仍可选用,但我国指南指出必须遵循优化治疗原则,严密监测,一旦耐药发生,应及时加用无交叉耐药的药物。新版指南则进一步强调,如初治应用LAM、ADV或LdT,在3个月发生原发性治疗无应答或6个月应答不佳者应停药,并换用更强药物或合并无交叉耐药的药物。
ETV相关临床数据
由于TDF用于慢性乙肝抗病毒治疗的适应证尚未在我国获批,因此对ETV的了解和临床应用数据格外令人关注。ETV Ⅲ期临床研究数据显示,治疗5年HBV DNA<300 copies/ml 的患者比例高达94%;亚太地区临床实践数据显示,ETV 0.5 mg治疗3年后,24%~44% 的患者出现 HBeAg转换,83%~90% 的患者HBV DNA不可测;即使对于治疗48周部分病毒学应答患者,继续ETV治疗,96周时高达81%的患者可达到HBV DNA 水平不可测,且无耐药发生。ETV具有高耐药基因屏障,其全球试验结果显示6年累计耐药发生率仅为1.2%(非ITT数据),日本和香港的数据显示ETV治疗3~5年的耐药发生率为0.6%~1.7%(ITT数据)。此外,ETV用于失代偿性肝硬化和慢加急CHB患者治疗时均表现了良好的耐受性。
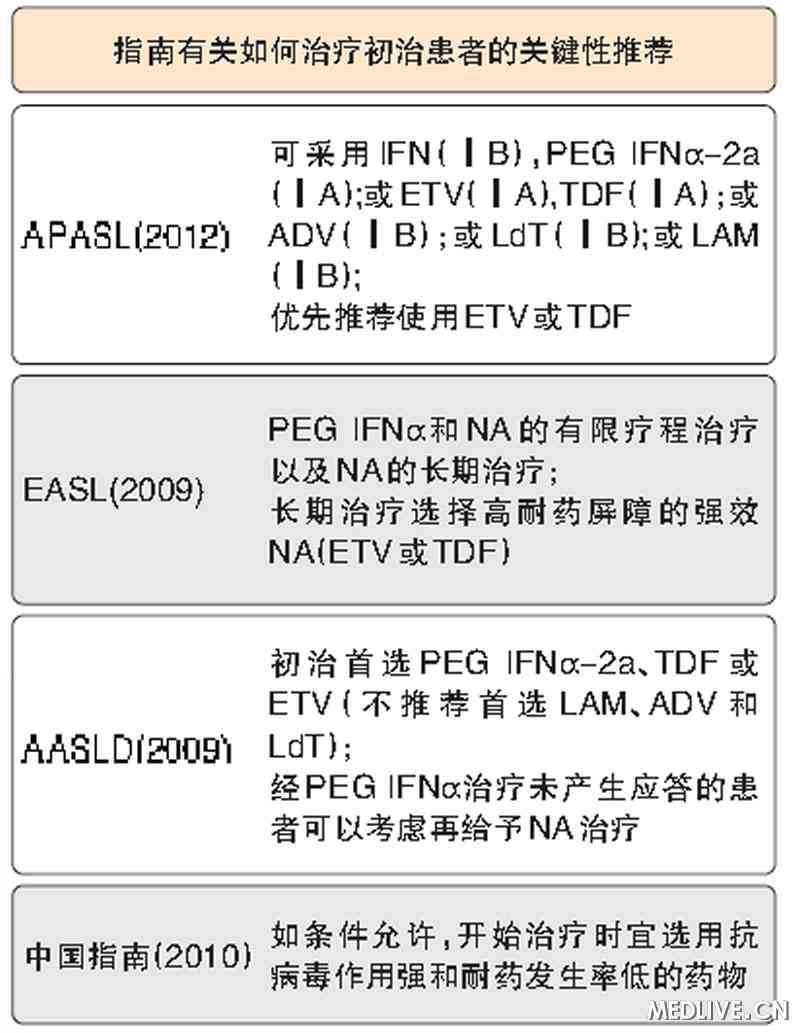
图 各国关于慢性乙肝初始治疗的对比分析
美国肝病研究学会(AASLD)、欧洲肝脏研究学会(EASL)指南均强调,基于达到长期治疗目标的需要,无论对CHB还是肝硬化患者,推荐首选强效、低耐药药物如ETV和TDF。我国《慢性乙型肝炎治疗指南》明确指出,如条件许可,初始宜选择抗病毒能力强和耐药发生率低的药物(表)。这充分表明,在初始药物选择方面,我国指南和APASL 2012版指南与国际主流观点趋于一致。初始选择强效低耐药药物是达到CHB长期治疗目标的重要手段。
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#药物选择#
28
#APA#
0
#CHB#
36
#ASL#
24
#APASL#
31