JAMA Neurol:睡眠不足可导致认知正常老年人Aβ负担加重,认知能力下降
2021-09-07 MedSci原创 MedSci原创
对于老年人群,睡眠不足可导致Aβ负担加重;过长或较短的睡眠时间与老年人抑郁、体重增加以及认知能力下降相关

衰老过程中由于生活方式和潜在的神经生理机制的变化导致老年人群的睡眠习惯出现显著变化,睡眠健康对衰老过程有重要的影响,而睡眠中断与抑郁、认知衰退、阿尔茨海默病(AD)以及心血管和代谢疾病风险增加有关。近日研究人员考察了自我报告的睡眠时间对认知能力正常的成人的大脑Aβ负担的影响。

本次研究在美国、加拿大、澳大利亚和日本的67个医疗中心进行,65至85岁志愿者接受PET-CT扫描和载脂蛋白e(apoe)基因型分析,参与者无痴呆症状,认知正常,自我报告夜间睡眠时间,按短睡眠时间分为睡眠不足(≤6小时),正常睡眠(7-8小时)以及睡眠时间长(≥9小时)。研究的主要终点为睡眠时间对人口统计学特征、Aβ负担、主客观认知以及生活方式的影响。
4417名志愿者参与研究,其中女性占59%,平均年龄71.3岁。研究发现,自我报告的睡眠时间缩短与Aβ负担增加线性相关(β=-0.01),与认知能力下降有关,其中对记忆相关领域的影响最显著。正常或较长时间睡眠不会导致Aβ负担变化,但相比于正常的睡眠时间,睡眠时间缩短或延迟导致体重指数增加、抑郁症状加重以及白天打盹现象。长时间睡眠与多个认知领域表现较差有关。
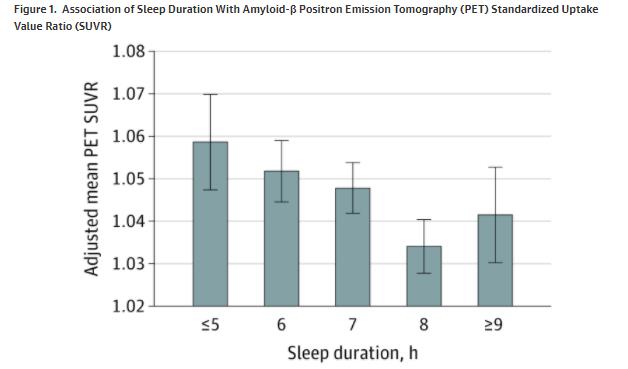
睡眠时间与Aβ负担
研究发现,对于老年人群,睡眠不足可导致Aβ负担加重;过长或较短的睡眠时间与老年人抑郁、体重增加以及认知能力下降相关。
原始出处:
Joseph R. Winer et al. Association of Short and Long Sleep Duration With Amyloid-β Burden and Cognition in Agingl. JAMA Neurol. August 30, 2021
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Neurol#
0
#认知能力下降#
44
#Aβ#
38
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
66
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
71