NEJM:在外科手术后利伐沙班在预防VTE方面优于依诺肝素(PRONOMOS研究)
2020-04-05 MedSci MedSci原创
发表在《新英格兰医学杂志》上的最新临床研究PRONOMOS,利伐沙班比依诺肝素在预防静脉血栓栓塞(VTE)事件更有效,而不会增加非重大下肢手术后制动患者的出血风险。该研究成果也在最近的ACC 2020
发表在《新英格兰医学杂志》上的最新临床研究PRONOMOS,利伐沙班比依诺肝素在预防静脉血栓栓塞(VTE)事件更有效,而不会增加非重大下肢手术后制动患者的出血风险。该研究成果也在最近的ACC 2020会议上公布。
这项国际双盲、随机对照试验首次在该中等风险人群中比较了口服利伐沙班与皮下注射依诺肝素。非劣效性试验计划测试利伐沙班是否不劣于依诺肝素。由于招募速度慢于预期,该试验于2018年4月早期终止,导致研究药物的有效期到了,而且替换药物的成本过高。在试验终止时,数据处于双盲状态。
研究人员研究了来自10个国家/地区的3,604名患者,被认为处于手术后VTE中等风险。他们被随机分到利伐沙班10 mg(1,809例)或依诺肝素4,000 IU(1,795例)。他们的中位年龄为41岁,三分之二是男性。总体而言,患者活动受限的中位时间为28天。
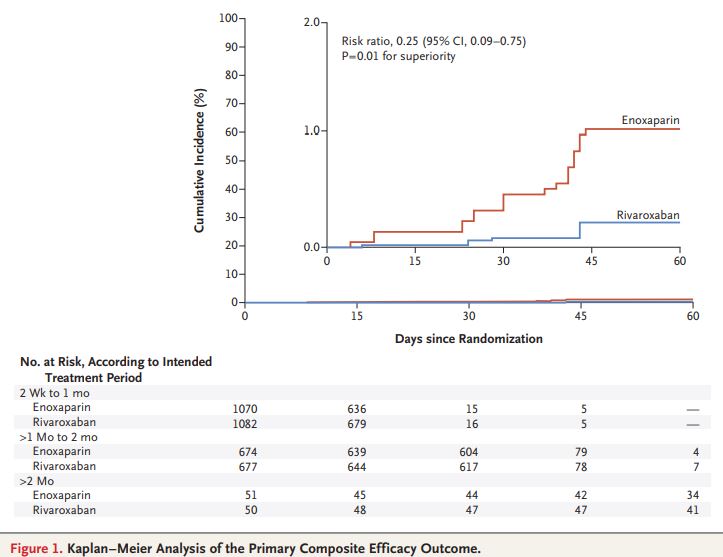
主要终点为主要VTE,包括治疗期间有症状的远端或近端深静脉血栓形成(DVT)、肺栓塞或VTE相关的死亡或无症状的近端DVT。
共有3604名患者接受了随机化治疗;1809名患者被分配接受利伐沙班,1795名患者接受依诺肝素。在主要终点方面,利伐沙班组1661名患者发生4例(0.2%),而依诺肝素组1,640例患者发生18例(1.1%)(多重填补的风险比,0.25;95%置信区间0.09-0.75;非劣效性p <0.001;优效性p = 0.01)。利伐沙班组与依诺肝素组的出血发生率无明显差异(严重出血或非严重临床相关的出血分别为1.1%和1.0%;严重出血分别为0.6%和0.7%)。
“在欧洲,所有指南都建议应给予一定程度的血栓预防措施,但总体而言,对于因在康复过程中被固定而仍处于中度血凝风险的患者人群应该采取的措施尚无共识。”研究者Nadia Rosencher博士说。“这项研究代表了我们在许多外科手术之后对患者进行治疗的重要一步,因为它证明,与安全性相同的每日注射相比,每日1次口服药物可以更有效地预防血栓形成。”
原始出处:
Samama CM, Laporte S, Rosencher N, Girard P, Llau J, Mouret P, Fisher W, Martínez-Martín J, Duverger D, Deygas B, Presles E, Cucherat M, Mismetti P; PRONOMOS Investigators.Rivaroxaban or Enoxaparin in Nonmajor Orthopedic Surgery.N Engl J Med. 2020 Mar 29. doi: 10.1056/NEJMoa1913808.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








学习了
103
#外科手术#
57
#依诺肝素#
46
#PRO#
41
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
65
学习了很有用不错
82