JCEM:TSH–FT4之间不是负对数线性关系
2013-05-27 JCEM dxy
甲状腺功能减退患者TSH中位数的分布 以往认为TSH与T4之间呈负对数线性关系,但是近来有研究挑战了这个观点。在TSH–T4关系中关注年龄和性别差异的数据有限。为了评估大样本人群中TSH–游离T4的关系,来自澳大利亚西澳大学查尔斯·盖尔德纳爵士医院John Walsh教授及其团队进行了一项研究,该研究发现TSH–游离T4不是负对数线性关系,但可以被两条重叠的负S行曲线所描述。在生理游离T4浓度下
以往认为TSH与T4之间呈负对数线性关系,但是近来有研究挑战了这个观点。在TSH–T4关系中关注年龄和性别差异的数据有限。为了评估大样本人群中TSH–游离T4的关系,来自澳大利亚西澳大学查尔斯·盖尔德纳爵士医院John Walsh教授及其团队进行了一项研究,该研究发现TSH–游离T4不是负对数线性关系,但可以被两条重叠的负S行曲线所描述。在生理游离T4浓度下,TSH在男性和老年人中比较高,然而,在年轻人中,TSH对甲状腺功能减退的反应更强烈。这些结果进一步认识了TSH–游离T4的关系,这对甲状腺疾病的甲状腺病理生理和实验室诊断极为重要。该研究结果在线发表在2013年5月13的美国《临床内分泌代谢杂志》(The journal of clinical endocrinology & metabolism)上。
该研究是一项横断面、回顾性研究,分析了来自单个实验室超过12年期间收集的152261受试者的TSH和游离T4。对每一个游离T4值(pmol/l),计算TSH中位数,并通过性别和年龄进行分析。
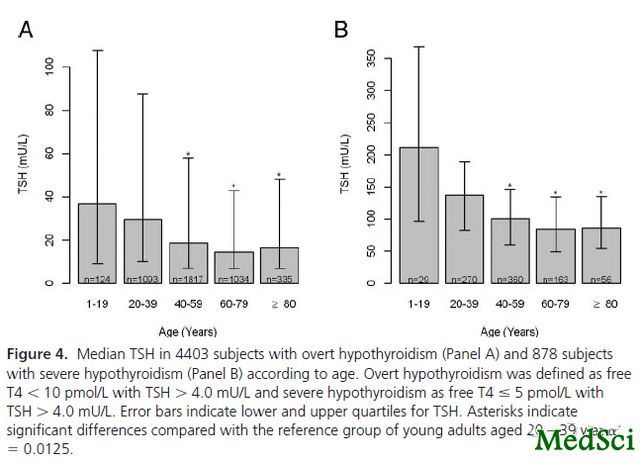
该研究结果表明,TSH对数与游离T4之间的关系是非线性的。数字模型确认两者之间的关系可被两条拐点在游离T4浓度为7和21pmol/l的S型曲线所描述。当游离T4在参考范围(10–20pmol/l)时,TSH的中位数在男性高于女性(P<0.001),并随着年龄而增加,在年龄超过80岁的受试者中到达最高值(P<0.001)。相比之下,在临床甲状腺功能减退的受试者中,相较于年龄20–39岁的受试者,在年龄较大者TSH比较低(P<0.001)。
该研究发现,TSH–游离T4不是负对数线性关系,但可以被两条重叠的负S行曲线所描述。在生理游离T4浓度下,TSH在男性和老年人中比较高,然而,在年轻人中,TSH对甲状腺功能减退的反应更强烈。这些结果进一步认识了TSH–游离T4的关系,这对甲状腺疾病的甲状腺病理生理和实验室诊断极为重要。

The relationship between TSH and free T4 in a large population is complex, non-linear and differs by age and gender.
Context
The relationship between TSH and T4 is thought to be inverse log-linear, but recent studies have challenged this. There are limited data regarding age and gender differences in the TSH-T4 relationship.Objective:To evaluate the TSH-free T4 relationship in a large sample.
Methods
In a cross-sectional, retrospective study we analyzed TSH and free T4 results from 152,261 subjects collected over 12 years by a single laboratory. For each free T4 value (in pmol/L), the median TSH was calculated and analyzed by gender and age (in 20 year bands).
Results
The relationship between log TSH and free T4 was nonlinear. Mathematical modeling confirmed that it was described by two sigmoid curves with inflexion points at free T4 concentrations of 7 and 21 pmol/L. For free T4 within the reference range (10 - 20 pmol/L), median TSH was higher in males than females (p<0.001) and increased across age bands with the highest values in those aged over 80 years (p<0.001). By contrast, in overt hypothyroidism (n= 4403), TSH was lower in older age groups compared with those aged 20 to 39 years (p<0.001).
Conclusions
The TSH-free T4 relationship is not inverse log-linear but can be described by two overlapping negative sigmoid curves. At physiological free T4 concentrations, TSH is higher in males and in older people, whereas the TSH response to hypothyroidism is more robust in younger people. These results advance understanding of the TSH-free T4 relationship, which is central to thyroid pathophysiology and laboratory diagnosis of thyroid disease.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#JCEM#
30
#JCE#
27
#TSH#
35