Eur Radiol:影像学上除了磁共振能够评估胰腺分泌功能,还有别的方法吗?
2017-12-06 shaosai MedSci原创
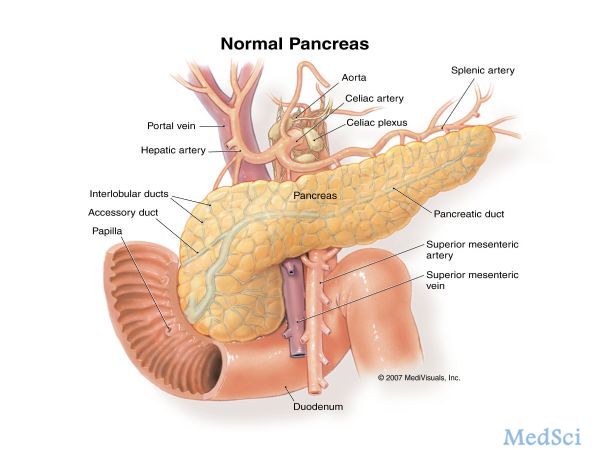
胰液分泌刺激磁共振(s-MRI)是评估胰腺分泌的最佳影像学检查方法。本研究旨在比较胰腺分泌刺激经腹超声(s-US)与s-MRI测量的分泌量在诊断囊肿纤维症(CF)患者胰腺外分泌机能不全的价值,并将结果发表在Eur Radiol上。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#分泌#
28
学习并分享!!
53
学习了.谢谢分享!
73
#磁共振#
27
学习学习.了解了解
61