Circulation:英国经导管主动脉瓣植入术后结局分析:长期结局得到改善,出院时间提前
2015-02-04 MedSci MedSci原创
近年来,主动脉瓣狭窄治疗中,经导管主动脉瓣植入术从一项新技术发展为目前的主流治疗。不过,对于术后长期结局仍旧缺乏有力的数据。英国伯明翰市伊利沙伯医院Ludman PF等人,自2007年至2012年,对3980例英国注册经导管主动脉瓣植入术的患者,评估了其临床特点,术后结局等指标。研究成果发表在1月份Circulation期刊上。 背景:研究评估了2007年至2012年英国首发病例经导管主动脉瓣植
近年来,主动脉瓣狭窄治疗中,经导管主动脉瓣植入术从一项新技术发展为目前的主流治疗。不过,对于术后长期结局仍旧缺乏有力的数据。英国伯明翰市伊利沙伯医院Ludman PF等人,自2007年至2012年,对3980例英国注册经导管主动脉瓣植入术的患者,评估了其临床特点,术后结局等指标。研究成果发表在1月份Circulation期刊上。
背景:研究评估了2007年至2012年英国首发病例经导管主动脉瓣植入术的趋势。分析了病例组合,并发症,术后六年结局和死亡率预测的变化。
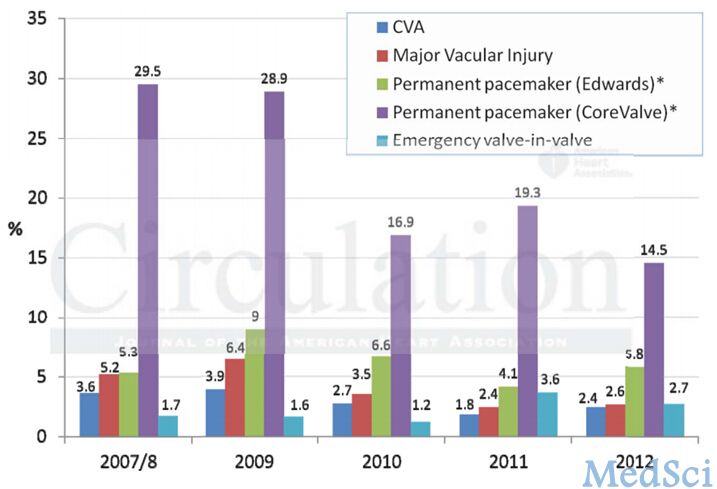
方法和结果:对每年的队列进行检查。分析了英格兰和威尔士92%的患者(可追踪独立死亡的患者)的死亡率。研究发现连续几年,左心室功能受损的频率增加了,但是EuroSCORE风险评分尚未改变。总体30天死亡率为6.3%;第一批队列30天死亡率最高(2007年8月),之后并没有进一步明显的改变。1年生存率为81.7%,在第6年的时候,生存率降到了37.3%。2007年8月5天出院率为16.7%,2012年上升为28%。30天死亡率的唯一多元预测因子是LES ≥ 40 。在长期随访中发现,死亡率的多元预测因子为术前房颤,慢性阻塞性肺病,肌酐> 200 µmol/l,糖尿病以及冠心病。长期死亡率最强的独立预测因子是围手术期发生脑卒中(HR=3.00,p<0.0001)。非股静脉通路和栓塞后主动脉返流也是不良结局的显著预测因子。
结局:在全国分析了经导管主动脉瓣植入术的长期结局,进行了为期6年的随访。尽管入选患者的临特点仍旧未改变,但术后长期结局结局还是有所改善,患者出院时间也得到了提前。围手术期卒中,非股静脉通路以及栓塞后主动脉返流都是不良结局的预测因子。
原始出处:
Ludman PF, Moat N, de Belder MA, Blackman DJ, Duncan A, Banya W, MacCarthy PA, Cunningham D, Wendler O, Marlee D, Hildick-Smith D, Young CP, Kovac J, Uren NG, Spyt T, Trivedi U, Howell J, Gray H. Transcatheter Aortic Valve Implantation in the UK: Temporal Trends, Predictors of Outcome and 6 Year Follow Up: A Report from the UK TAVI Registry 2007 to 2012. Circulation. 2015.
本文是MedSci编译,欢迎转载,转载请注明出处,非常感谢!

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#经导管主动脉瓣植入#
23
#主动脉瓣植入术#
30
已阅
92
小编评论亮了
84
#主动脉瓣#
29
#长期结局#
33
#主动脉#
34
#经导管#
35
#植入#
19
good !
119