Hypertension:脉压和动脉硬度对心血管疾病的相对作用
2019-01-21 xing.T MedSci原创
由此可见,该研究的结果表明脉压-动脉僵硬度不匹配在社区人群中很常见。CFPWV可能会改变CPP与CVD风险之间的关联,在CPP和CFPWV升高的患者中观察到的风险最大。
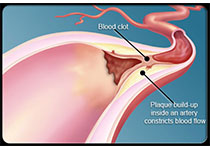
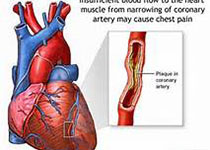
脉压经常被用作动脉顺应性的替代标志。然而,脉压与动脉僵硬度不匹配的患病率和预后意义尚不清楚。近日,心血管权威杂志Hypertension上发表了一篇研究文章,研究人员测量了Framingham后代队列中2119名参与者(平均年龄为60岁; 57%为女性)的颈动脉-股动脉脉搏波速度(CFPWV)和中心脉压(CPP)。
参与者根据CPP和CFPWV状态分为4组(根据年龄和性别特异性中位数分类为高/低两类)并对心血管疾病(CVD)事件进行随访。
在基线时,2119名(39%)参与者中有832人具有不一致的CPP和CFPWV状态,417人具有低CPP和高CFPWV,415人具有高CPP和低CFPWV。CPP-CFPWV不匹配患者CVD事件的多变量调整风险(n=246;中位随访12.6年)(低CPP与高CFPWV的风险比为1.21; 95%CI为0.83-1.76;高CPP与低CFPWV的风险比为0.76; 95%CI为0.49-1.19)与低CPP和低CFPWV患者(参考组)中观察到的CVD风险相当。相反,具有高CFPWV和高CPP(风险比为1.52; 95%CI为1.10-2.11)的参与者经历CVD风险显著增加。CPP和CFPWV状态对CVD风险的相互作用在多变量模型中具有临界意义(P=0.08)。
由此可见,该研究的结果表明脉压-动脉僵硬度不匹配在社区人群中很常见。CFPWV可能会改变CPP与CVD风险之间的关联,在CPP和CFPWV升高的患者中观察到的风险最大。
原始出处:
Teemu J. Niiranen.et al.Relative Contributions of Pulse Pressure and Arterial Stiffness to Cardiovascular Disease The Framingham Heart Study.Hypertension.2019.https://www.ahajournals.org/doi/10.1161/HYPERTENSIONAHA.118.12289
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#PE#
47
#相对作用#
42
#动脉硬度#
43
#TENS#
40
#血管疾病#
0
#Hypertension#
42