Sci Signal:乳腺癌细胞代谢异常研究新突破
2017-12-26 陈扬 “医海拾贝微转化”微信号
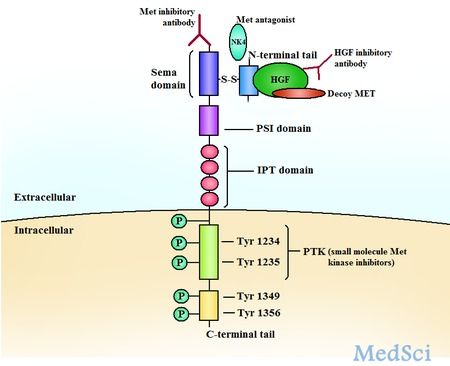
甲硫氨酸(Met)依赖性是肿瘤细胞代谢异常的重要特征之一。所谓肿瘤Met依赖性是指与相应正常组织细胞不同,肿瘤细胞在去除Met(又称Met限制)的环境中 (即用Met的前体物质同型半胱氨酸取代Met)无法生长 。近日来自哈佛大学的一项研究发表在《Science Signaling》,揭示了因PI3KCA基因突变而驱动的乳腺癌,可抑制胱氨酸转运通道,而导致癌细胞对Met的依赖。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#Sign#
33
#Signal#
33
#新突破#
35
学习了谢谢作者分享!
44
#癌细胞#
29
#细胞代谢#
27
#代谢异常#
36