Neurology:CADASIL患者血管认知功能障碍的患病率及预测因素
2022-07-11 Naomi MedSci原创
伴有皮质下梗塞和白质脑病的常染色体显性遗传性脑动脉病是最常见卒中遗传形式。研究发现轻度认知障碍存在于近一半平均年龄50岁的CADASIL患者群体中,卒中和MRI腔隙数是BMET上VCI的独立预测因素。
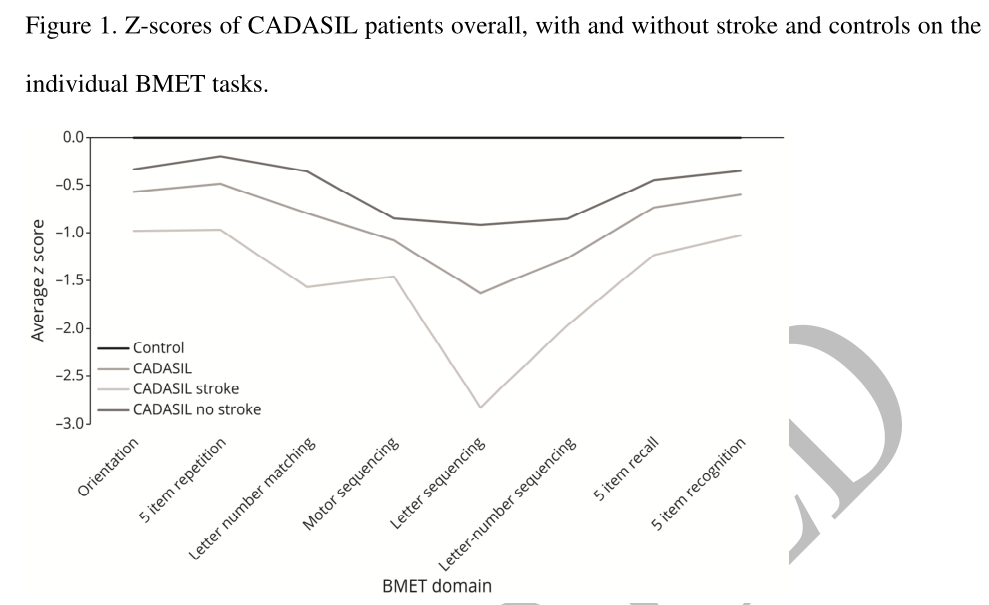
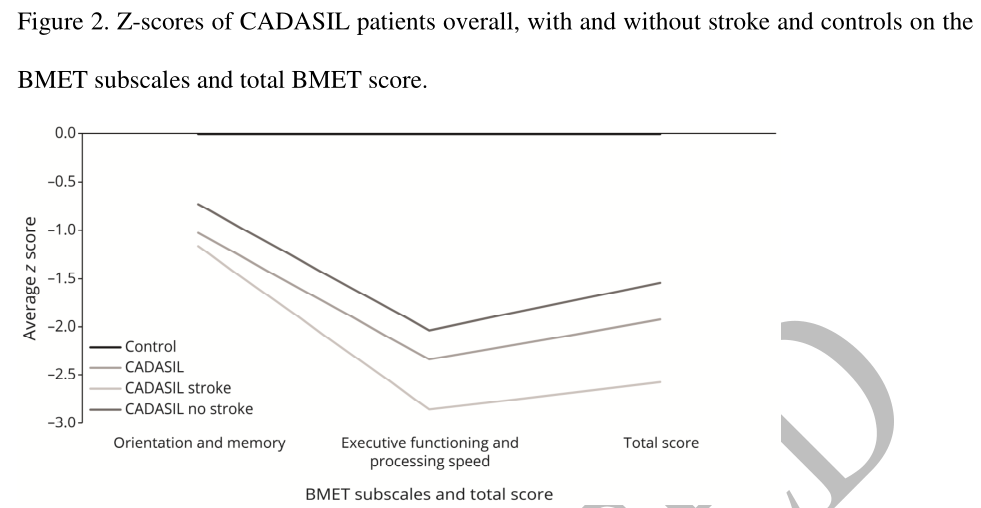
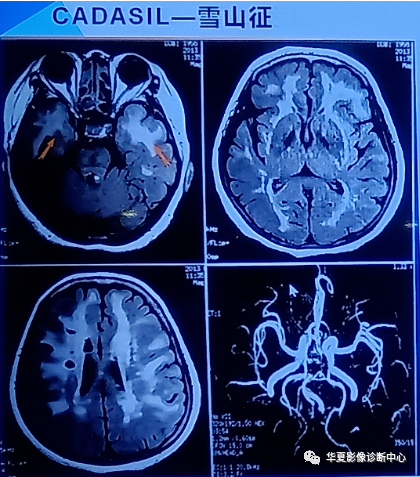
CADASIL(伴有皮质下梗塞和白质脑病的常染色体显性遗传性脑动脉病)是卒中最常见的遗传形式。NOTCH3基因的突变导致一种小血管动脉病变,临床特征为早发性卒中、血管认知障碍和痴呆。虽然大多数有症状的患者在以后的几年中会表现出一些认知障碍,疾病的病程和严重程度在个人之间甚至在家庭内都是非常不同的,其原因尚不确定。虽然血管风险因素与进展更快有关,而且最近突变部位与严重程度有关,更多的近端突变导致更早的卒中发作。先前的研究表明,CADASIL认知障碍的早期特征包括执行功能障碍和信息处理速度减慢,对工作记忆和情景长期记忆的早期影响不太一致。以前在CADASIL中进行的大多数认知研究都是小规模或中等规模的。
CADASIL是卒中和早发性痴呆最常见的单基因形式。近日,一项发表在Neurology上的研究确定了一组CADASIL患者中血管认知损害(VCI)的患病率,并调查了哪些因素与VCI风险相关,包括临床、遗传和MRI参数。
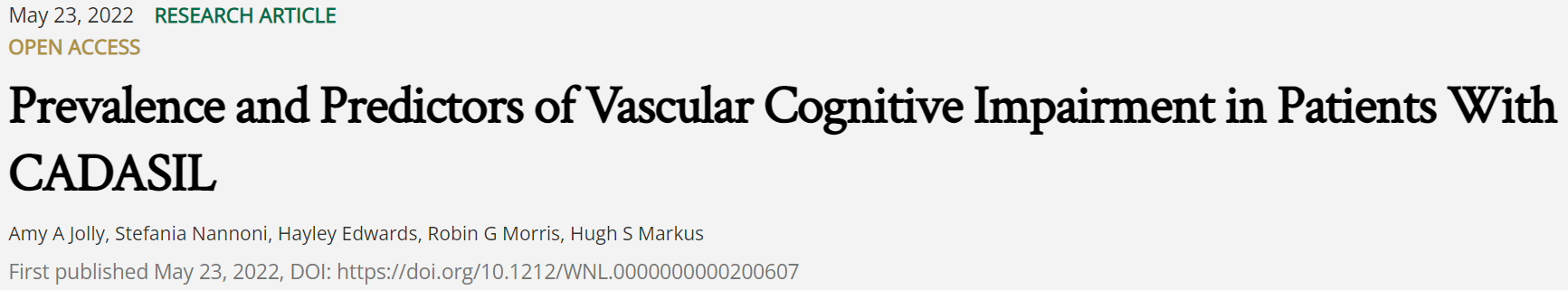
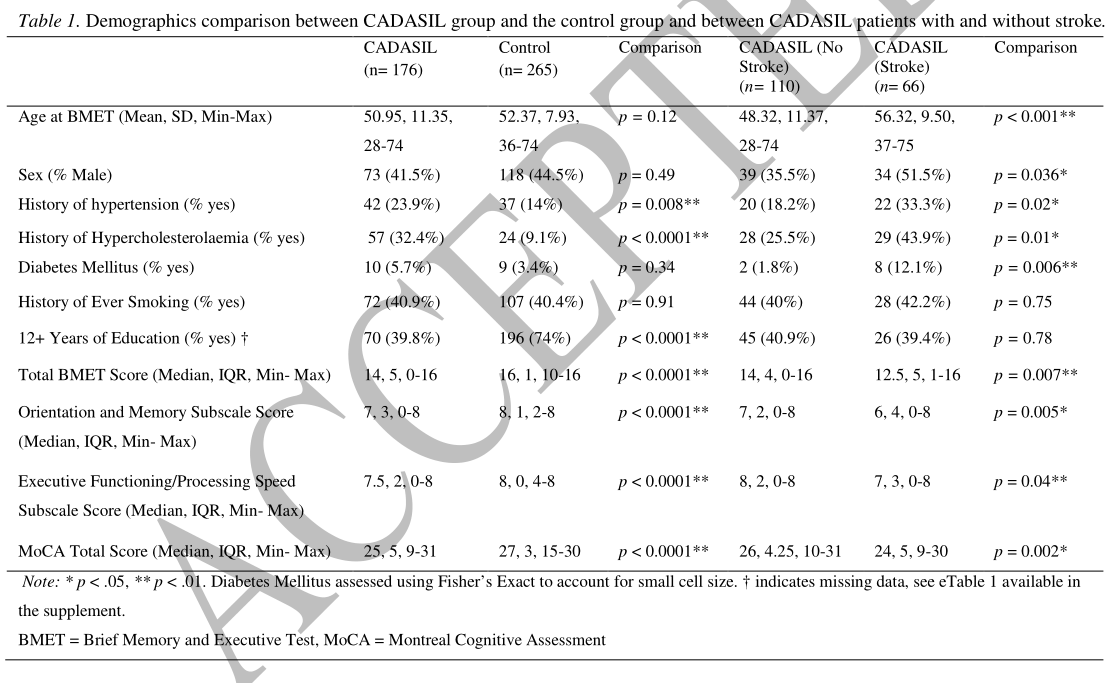
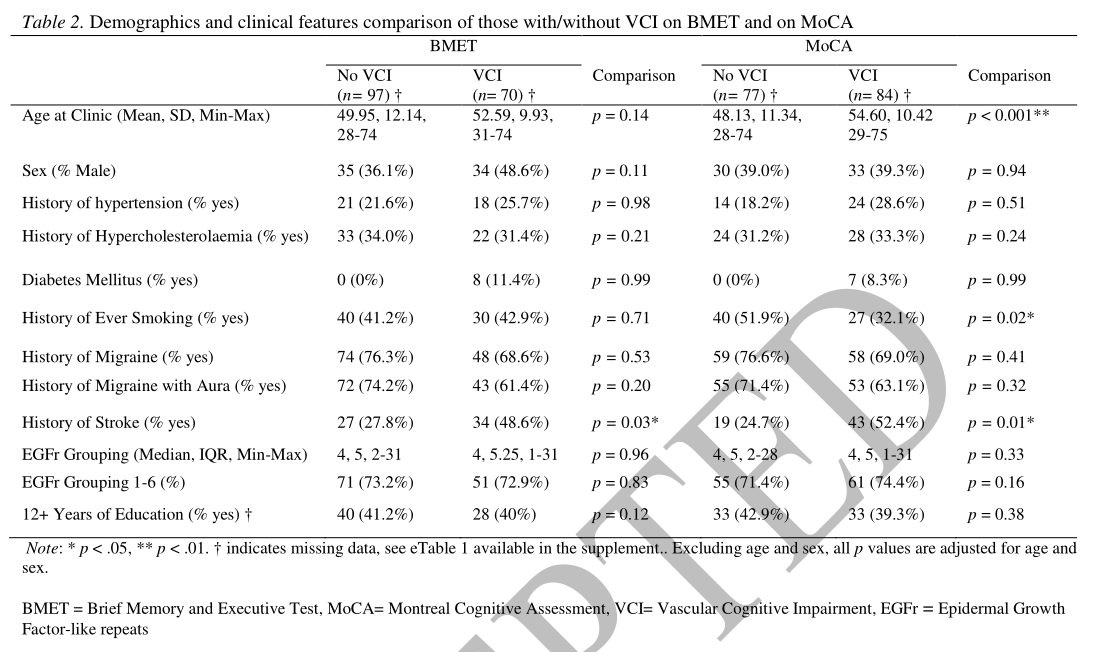
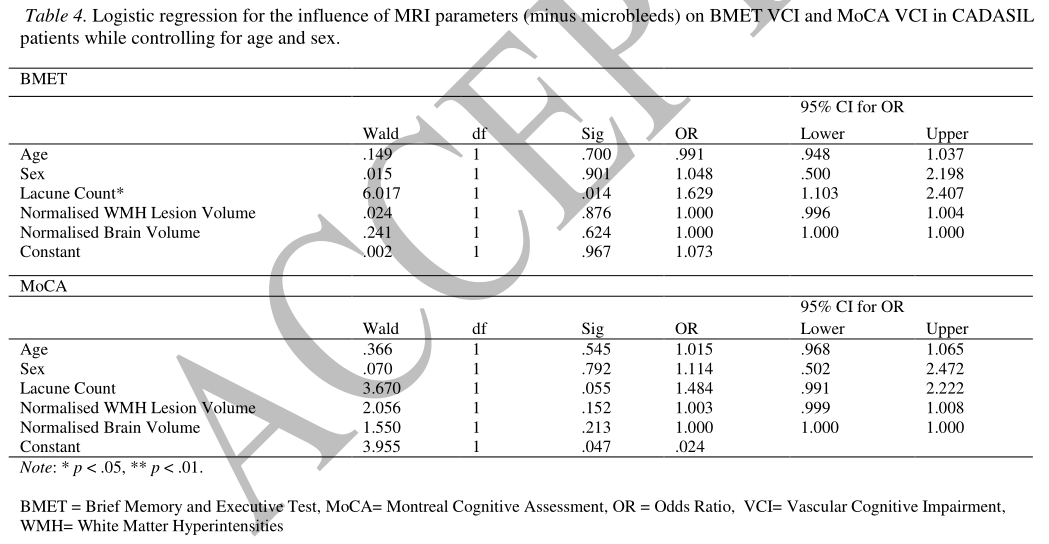
对176例遗传确诊的CADASIL患者和265例健康对照(平均年龄50.95岁(11.35岁)对52.37岁(7.93岁))的认知能力进行了评估,使用简短记忆和执行测试(BMET)和蒙特利尔认知评估(MoCA)。VCI是根据先前验证的截断值定义的。我们确定了VCI的患病率及其与临床危险因素、突变位置(EGFR 1-6与EGFR 7-34)以及小血管疾病的MRI标志物的关系。
- CADASIL组VCI发生率高于对照组,BMET组39.8%,MOCA组47.7%,MOCA组19.6%。CADASIL患者在所有认知领域的表现都较差。
- 在控制年龄和性别后,卒中病史与BMET(OR 2.12,95%CI[1.05,4.27]p=0.04)和MoCA(OR 2.55[1.21,5.41]p=0.01)的VCI相关。未发现VCI与突变位点相关。
- 在控制其他磁共振参数后,腔隙数是唯一与BMET上的VCI独立相关的磁共振参数(OR:1.63,95%CI[1.10,2.41],p=0.014)。
- 在敏感性分析中控制了教育因素后,这些关联仍然存在。
VCI存在于平均年龄为50岁的CADASIL患者中的近一半。卒中和MRI上的腔隙数都是BMET上VCI的独立预测因素。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#CADASIL#
28
#Neurol#
34
#患病率#
48
#预测因素#
39
#ADA#
38
#功能障碍#
57