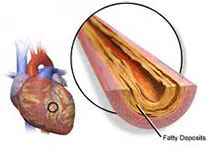
Diabetologia:犬尿氨酸:色氨酸比例作为冠状动脉疾病患者2型糖尿病预测因子
2017-09-30 MedSci MedSci原创
近日,国际杂志 《Diabetologia》上在线发表一项关于犬尿氨酸:色氨酸比例作为冠状动脉疾病患者2型糖尿病预测因子的研究。
近日,国际杂志 《Diabetologia》上在线发表一项关于犬尿氨酸:色氨酸比例作为冠状动脉疾病患者2型糖尿病预测因子的研究。 色氨酸代谢物犬尿氨酸具有很强的免疫调节和血管活性。实验数据表明犬尿氨酸与肥胖病态相关。但关于其的流行病学研究却很少。研究人员评估了血浆和尿液犬尿氨酸:色氨酸比(KTR)与2型糖尿病的关联性。 研究人员跟踪了中位数为7.6年共2519无基础糖尿病的冠状动脉疾病患者(CAD;男性占73.1%),期间确定了173例(6.9%)新发生的2型糖尿病。应用多因素Cox回归分析来研究血浆和尿KTR与新发2型糖尿病的前瞻性关系。 研究结果显示,研究群体平均(SD)年龄为61.3(10.4)岁,BMI为25.9(3.71)kg/m 2,中位数(四分位数范围)HbA 1c为5.6%(5.0%-6.0%)(38 [31-42]mmol/mol)。血浆KTR与2型糖尿病风险无显著相关性。相比之下,尿KTR表现出强相关性。比较四分位数,HR(95%CI)分别在年龄和性别校正和多变量模型中分别为2.59(1.56,4.30)和2.35(1.39,3.96)。 研究表明,尿KTR是CAD
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#BET#
27
#疾病患者#
27
#DIA#
31
#冠状动脉疾病#
26
#预测因子#
31