Cancer Res.:陷窝蛋白-1调节大肠癌有氧糖酵解
2012-06-18 bo 生物谷
6月15日,Cancer Research杂志在线报道了在大肠癌中,陷窝蛋白-1通过刺激HMGA1介导的GLUT3转录,增加有氧糖酵解。 陷窝蛋白-1(CAV1)在多种人类恶性肿瘤中作为生长抑制因子,但在许多晚期癌症中其表达升高,提示其在肿瘤进展中的致癌开关作用。为理解CAV1增长促进作用的分子基础,研究者分析了其在肿瘤生长中的表达状态和在分化中的作用,以及它对大肠癌肿瘤的生长和糖代谢的影响。在
6月15日,Cancer Research杂志在线报道了在大肠癌中,陷窝蛋白-1通过刺激HMGA1介导的GLUT3转录,增加有氧糖酵解。
陷窝蛋白-1(CAV1)在多种人类恶性肿瘤中作为生长抑制因子,但在许多晚期癌症中其表达升高,提示其在肿瘤进展中的致癌开关作用。为理解CAV1增长促进作用的分子基础,研究者分析了其在肿瘤生长中的表达状态和在分化中的作用,以及它对大肠癌肿瘤的生长和糖代谢的影响。在很大一部分原发肿瘤和细胞系中,可检测到CAV1的异常升高。这与启动子CpG位点的低甲基化紧密相关。
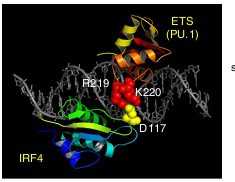
升高CAV1的消耗,导致AMPK活化和随后的p53依赖的G1细胞周期阻滞和细胞自噬。这表明升高CAV1可能促进ATP生成。此外,CAV1的消耗可下调葡萄糖的摄取,乳酸堆积和细胞内ATP水平。这提示,CAV1增强有氧糖酵解。相应的,研究结果表明CAV1通过一个GLUT3启动子内的HMGA1结合位点,刺激GLUT3的转录。
研究还发现,HMGA1与GLUT3启动子相互作用并活化它,而CAV1通过加强HMGA1的核定位来增加其活力。 HMGA1的异位表达增加葡萄糖的摄取,而其表达下调导致AMPK激活。此外,共转染CAV1和HMGA1可诱导GLUT3强烈表达。GLUT3过度表达主要表现在高水平表达CAV1和HMGA1的肿瘤中。总之,这些数据显示,升高的CAV1通过HMGA1介导的GLUT3转录上调葡萄糖的摄取和ATP的生产。这表明,CAV1提高有氧糖酵解可能导致肿瘤细胞的生长优势。

doi:10.1016/j.cell.2011.10.017
PMC:
PMID:
Caveolin-1 Increases Aerobic Glycolysis in Colorectal Cancers by Stimulating HMGA1-Mediated GLUT3 Transcription
Sung-Gil Chi1,*, Tae-Kyu Ha1, Nam-Gu Her1, Min-Goo Lee1, Byung-Kyu Ryu1, Jin-Hee Lee1, Jikhyon Han1, Seong-In Jeong1, Min-Ju Kang1, Nam-Hoon Kim2, and Hyo-Jong Kim3
Caveolin-1 (CAV1) acts as a growth suppressor in various human malignancies but its expression is elevated in many advanced cancers, suggesting the oncogenic switch of its role during tumor progression. To understand the molecular basis for the growth-promoting function of CAV1, we characterized its expression status, differential roles for tumor growth and effect on glucose metabolism in colorectal cancers. Abnormal elevation of CAV1 was detected in a substantial fraction of primary tumors and cell lines and tightly correlated with promoter CpG sites hypomethylation. Depletion of elevated CAV1 led to AMPK activation followed by a p53-dependent G1 cell cycle arrest and autophagy, suggesting that elevated CAV1 may contribute to ATP generation. Furthermore, CAV1 depletion down-regulated glucose uptake, lactate accumulation and intracellular ATP level, supporting that aerobic glycolysis is enhanced by CAV1. Consistently, CAV1 was shown to stimulate GLUT3 transcription via a HMGA1-binding site within the GLUT3 promoter. HMGA1 was found to interact with and activate the GLUT3 promoter and CAV1 increased the HMGA1 activity by enhancing its nuclear localization. Ectopic expression of HMGA1 increased glucose uptake while its knockdown caused AMPK activation. In addition, GLUT3 expression was strongly induced by co-transfection of CAV1 and HMGA1 and its overexpression was observed predominantly in tumors harboring high levels of CAV1 and HMGA1. Together, these data show that elevated CAV1 up-regulates glucose uptake and ATP production through HMGA1-mediated GLUT3 transcription, suggesting that CAV1 may render tumor cells growth advantages by enhancing aerobic glycolysis.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












又是糖酵解啊
81
#陷窝蛋白-1#
35
#Res.:#
35
#糖酵解#
54