Gene & Cancer Sci:重磅:盐酸安罗替尼抗血管生成机制详解
2018-04-03 肿瘤资讯编辑部 肿瘤资讯
近日,中国药科大学的卢娜教授和上海药物研究所的楼丽广教授分别在《Gene》和《Cancer Science》杂志在线发表两篇关于新型国产血管靶向药物盐酸安罗替尼的抗血管生成机制的研究论文,为其临床应用提供了翔实的理论依据,同时也给盐酸安罗替尼在其他肿瘤领域的探索提供了一些思路。
自上世纪70年代初,哈佛大学医学院教授,美国国家科学院院士Judah Folkman教授提出了著名的“饿死肿瘤疗法”理论,即通过阻断肿瘤新生血管生成切断肿瘤营养供给而达到抑制和治疗肿瘤的目的。经过近50年的发展,已有包括贝伐珠单抗(Avastin)雷莫卢单抗(Cyramza)两个抗体药物以及小分子血管靶向TKI,如舒尼替尼、索拉非尼、凡德他尼、帕唑帕尼和仑伐替尼等药物成功上市,应用于肾癌、软组织肉瘤、肝癌、肺癌等多个领域。然而,国内对此类药物的开发相对缓慢,目前上市的国产药物屈指可数。近日,中国药科大学的卢娜教授和上海药物研究所的楼丽广教授分别在《Gene》和《Cancer Science》杂志在线发表两篇关于新型国产血管靶向药物盐酸安罗替尼的抗血管生成机制的研究论文,为其临床应用提供了翔实的理论依据,同时也给盐酸安罗替尼在其他肿瘤领域的探索提供了一些思路。
一、盐酸安罗替尼能够强效抑制多个血管生成相关激酶和肿瘤生长相关激酶活性
众所周知,VEGFR、PDGFR和FGFR所介导的三条信号通路及其之间的Crosstalk是调控肿瘤血管新生的主要机制,而这其中又以VEGFR2所介导的信号通路最为重要,因此目前的血管靶向药物多以VEGFR2作为主要靶点。盐酸安罗替尼也不例外,对VEGFR2、VEGFR3的抑制活性最强,IC50分别为0.2nM和0.7nM。不仅如此,盐酸安罗替尼对于PDGFR和FGFR通路同样具有强烈的抑制作用。因此,相比其他抗血管生成药物,盐酸安罗替尼能够同时抑制血管形成相关的三条信号通路,全面阻断肿瘤血管新生。此外,盐酸安罗替尼对于干细胞因子受体c-Kit也显示出了很强的抑制活性,c-Kit所介导的信号通路在多种恶性肿瘤的发生、发展以及复发的过程中扮演着重要角色,也是目前众多在研靶向药物的主要靶点。通过分子动力学模拟发现,盐酸安罗替尼主要结合在VEGFR2和c-Kit激酶的ATP结合域,和舒尼替尼相比,盐酸安罗替尼能够更深地进入ATP结合位点的催化口袋,其结构中的吲哚环恰好位于DFG-motif (天冬氨酸-苯丙氨酸-甘氨酸模段)附近,而DFG motif对于激酶活性具有重要的调控作用,盐酸安罗替尼可能通过和DFG motif 发生相互作用而显示出极强的激酶抑制活性。
体外激酶活性测定和分子动力学模拟结果提示,盐酸安罗替尼可能具有既能全面抑制肿瘤血管新生,也能通过c-Kit等激酶干预肿瘤细胞本身多个生物学过程的双重功能。
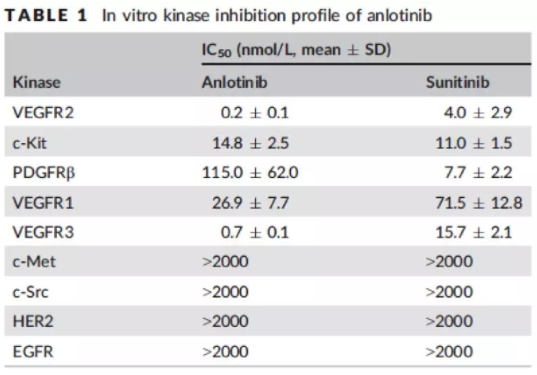
表1. 盐酸安罗替尼体外激酶抑制活性
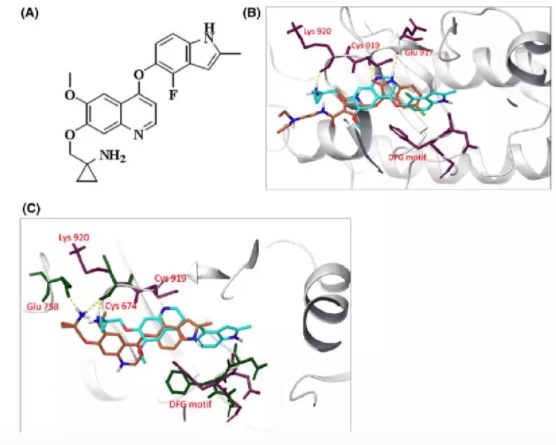
图1. 盐酸安罗替尼结合VEGFR2(A)和c-Kit(B)模式图,图中蓝色为盐酸安罗替尼,橘红色为舒尼替尼
二、盐酸安罗替尼抑制相关受体下游信号通路激活,阻断细胞增殖、迁移等多个生物学过程
与调控血管新生相关的主要三条信号通路之间存在着广泛的Crosstalk,各信号通路在下游的信号传递过程中可通过对ERK、Akt和PI3K等激酶的调控实现Crosstalk,这就意味着同时抑制VEGFR、PDGFR和FGFR介导的三条信号通路相比单纯抑制其中某一条信号通路而言,发生旁路激活而重新启动血管新生的可能性更低,作用更为全面。
Western Blot试验证实(图2),盐酸安罗替尼能够显著抑制VEGFR2、c-KIT、PDGFRβ等激酶的磷酸化,进而抑制其下游信号通路中ERK及Akt等激酶的磷酸化,有效阻断其相关信号通路。而对于EGFR和HER2等激酶,在相同的试验浓度(0.1-1000 nM)下,则没有观察到显著的抑制作用,说明盐酸安罗替尼对于血管形成相关受体以及c-Kit具有较强的选择性。能够特异性地结合血管新生相关的受体,有效阻断其信号传导,从而发挥抗血管生成的作用。

图2. 盐酸安罗替尼对相关信号通路及其下游信号通路的抑制作用
如图3所示,通过细胞水平及组织水平的研究发现,经过盐酸安罗替尼处理,VEGF刺激的人脐静脉内皮细胞(HUVEC)的增殖能力显著下降。通过划痕愈伤试验发现,由VEGF/PDGF-BB/FGF-2介导的内皮细胞发生迁移的能力也明显降低,在同个试验浓度下,盐酸安罗替尼的效果显著强于对照药物。Transwell小室试验的结果和愈伤试验一致,在VEGF、FGF及PDGF等相应细胞因子刺激下,盐酸安罗替尼均能够有效的抑制内皮细胞发生迁移,且抑制效率显著优于对照药物。
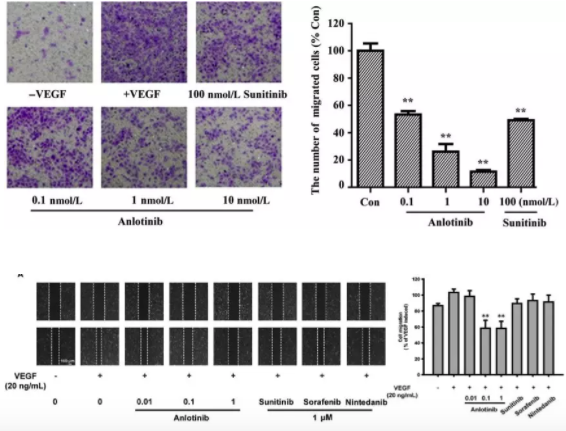
图3. 盐酸安罗替尼对新生血管的抑制作用(**P<.01)
在组织水平上(图4),大鼠动脉环和微管形成试验均发现,盐酸安罗替尼能够有效抑制新生血管的形成。大鼠动脉环试验发现,盐酸安罗替尼在10nM水平就能够有效抑制约80%的新生微血管形成;微管形成试验发现,盐酸安罗替尼能够更有效的抑制HUVEC细胞形成管状结构。从而在组织和亚组织层面证实了盐酸安罗替尼抑制血管形成的功能。
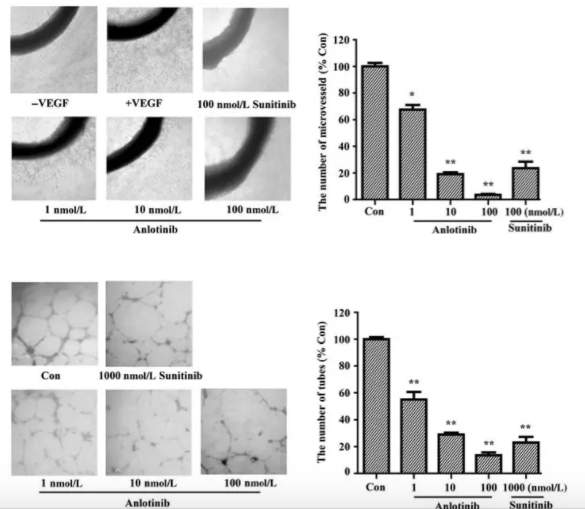
图4. 盐酸安罗替尼对新生血管的抑制作用(*P<.05,**P<.01)
三、盐酸安罗替尼能够显著降低荷瘤小鼠瘤体中的血管数量
通过SW620异种移植瘤模型研究发现,盐酸安罗替尼对移植瘤的抑制作用呈现明显的剂量依赖性,高剂量的盐酸安罗替尼(3mg/kg)处理后的瘤体,其体积均值仅为空白对照组的20%。观察瘤体内部发现,经过盐酸安罗替尼处理后的瘤体,其内部血管数量显著低于空白对照组,且试验组的动物并没有发生显著的体重下降。

图5. 盐酸安罗替尼小鼠移植瘤模型及瘤内血管密度
结语:
相继发表的两项机制研究证实,盐酸安罗替尼独特的分子结构决定了盐酸安罗替尼能够强烈抑制血管新生相关的VEGFR、FGFR及PDGFR所介导的下游信号通路,干预内皮细胞的增殖、迁移及形成管腔的能力,进而抑制微小血管的形成,并且能通过c-Kit激酶干预肿瘤细胞本身的多个生物学过程。动物试验发现,盐酸安罗替尼能够有效的抑制移植瘤的生长,显著降低瘤内微血管的数量。
原始出处:
【1】Binyan Lin, Xiuming Song, Dawei Yang, et al. Anlotinib inhibits angiogenesis via suppressing the activation of VEGFR2, PDGFRβ and FGFR1. Gene,654(2018), 77-86.
【2】Chengying Xie, Xiaozhe Wan, Haitian Quan, et al. Preclinical characterization of anlotinib, a highly potent and selective vascular endothelial growth factor receptor-2 inhibitor. Cancer Science, 2018:1-13.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言






#抗血管#
44
#Gene#
44
#盐酸安罗替尼#
47
#抗血管生成#
39
#重磅#
0
学习
63
谢谢分享学习了
74