Crit Care:瘦体重是重症监护病房入院的危险因素
2021-10-19 MedSci原创 MedSci原创
在这项基于人群的队列研究中,瘦体重与入住ICU无关;然而,更大的四肢瘦体重与死亡率降低相关。这表明入住ICU前肌肉状态可能无法预测危重疾病的发展,但与危重疾病发生后更好的生存相关。
重症监护病房(ICU)幸存者身体机能下降可能是由于骨骼肌萎缩和危重疾病期间虚弱所致。然而,尚未阐明病前肌肉质量的作用。

近日,危重病医学领域权威杂志Critical Care上发表了一篇研究文章,研究人员旨在评估ICU前肌肉质量与ICU入住风险之间的关联。次要结局包括肌肉质量与ICU结局之间的关系。

研究人员从基于人群的队列研究-吉朗骨质疏松症研究(GOS)的参与者中确定了1998年6月1日至2019年2月1日期间入住ICU的患者,并采用Cox比例风险回归模型估计了不同T分数层和DXA衍生的骨骼质量指数的瘦体重测量值(SMI,瘦体重/体重%)的连续值和针对身高校正的四肢瘦体重(ALM/h2,kg/m2)的个体入住ICU的风险比(HR)。多变量回归用于确定瘦体重与ICU结局之间的关系。
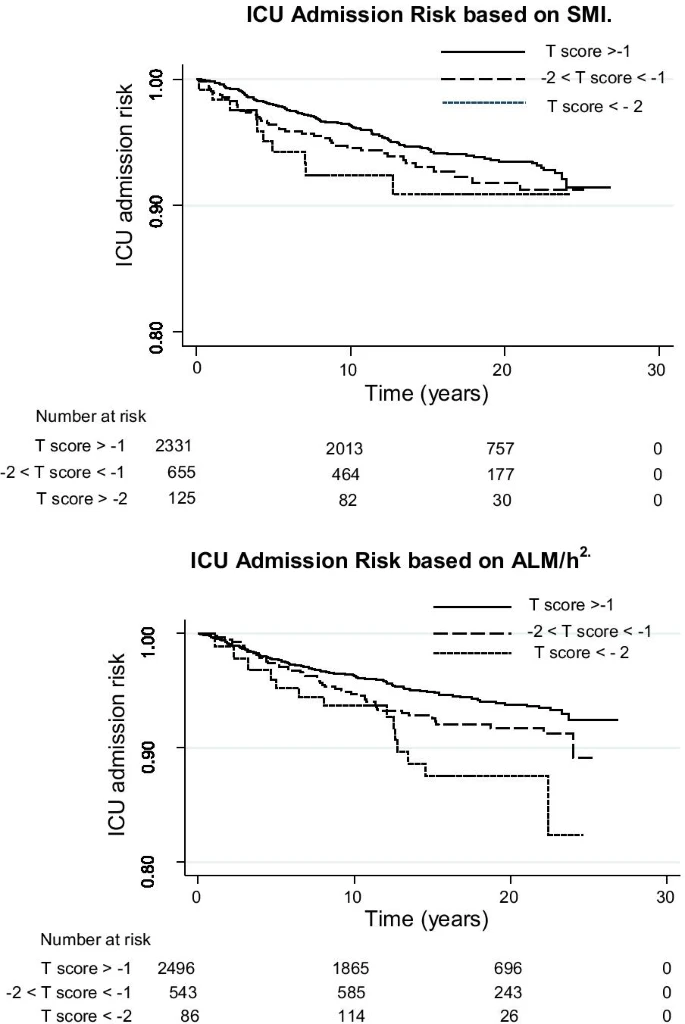
在随访期间,GOS登记的3126名参与者中有186名受试者入住ICU。在调整后的模型中,瘦体重不能预测入住ICU(SMI:HR为0.99,95%CI为0.97-1.01,p=0.32;ALM/h2:HR为1.11,95%CI为0.94-1.31,p=0.23),而四肢瘦体重更大与28天死亡率降低相关(ALM/h2,adjOR:0.25,95%CI为0.10-0.63,p=0.003,SMI,adjOR:0.91,95%CI为0.82-1.02,p=0.09)。
在这项基于人群的队列研究中,瘦体重与入住ICU无关;然而,更大的四肢瘦体重与死亡率降低相关。这表明入住ICU前肌肉状态可能无法预测危重疾病的发展,但与危重疾病发生后更好的生存相关。
原始出处:
Matthew Thackeray.et al.Lean mass as a risk factor for intensive care unit admission: an observational study.Critical Care.2021.https://ccforum.biomedcentral.com/articles/10.1186/s13054-021-03788-y
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#重症监护病房#
47
#监护#
37
👍。
64
不错,学习了。
59
学习
74
很不错哦 学习了
61