JACC:影响复苏抢救过的心脏骤停患者生存率的因素
2021-06-12 Nebula MedSci原创
心律失常原因、室性心动过速/纤颤初始节律和白种人都是复苏性心脏骤停患者存活的独立预测因素
在POST SCD研究中,研究人员解剖了大量世界卫生组织(WHO)定义的心源性猝死(SCD)病例,发现只有56%的病例是死于心律失常;复苏性心脏骤停(SCA)个体因不是猝死而被排除在外。他们推测,导致SCA复苏的原因也可能具有类似的异质性。
本研究目的是确定复苏性SCA病例的发病原因和临床预后。
该研究纳入了2011年2月1日至2015年1月1日在旧金山发生的所有18-90岁的院外心脏骤停(OHCA)患者。复苏性SCAs是指活到住院并符合WHO意外标准的OHCA。通过全面的病厉审查确定发病原因。
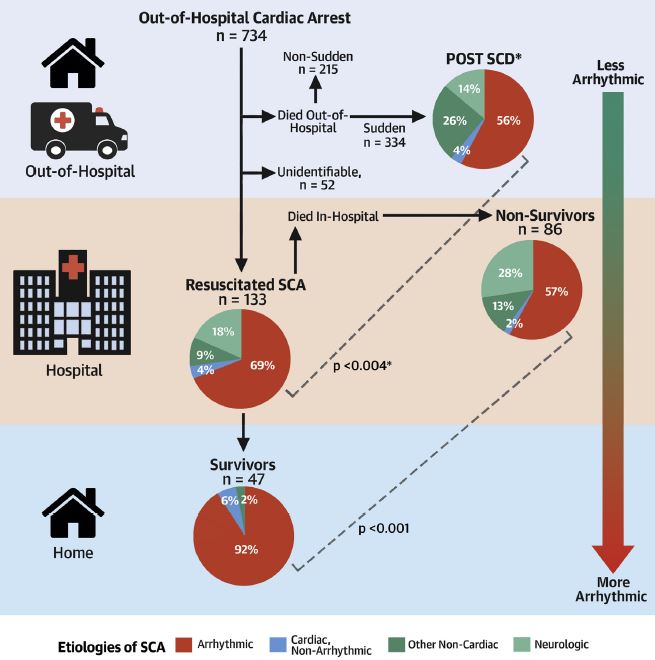
存活情况不同的患者的发病原因比例
48个月内,共鉴定出了734例OHCA,其中239人符合SCA标准,133人(55.6%)经复苏后活着入院,47人(19.7%)活着出院。总的来说,与WHO定义的SCD相比,可归因于心律失常的复苏性SCD患者比例更高(92/132[69.1%] vs 293/525[55.8%]),该比例在幸存者中明显更高(43/47,91.5%)(p<0.004)。
复苏性SCA患者的发病原因
对于复苏性SCA患者,心律失常原因、室性心动过速/纤颤初始节律和白种人都是存活的独立预测因素。因神经系统原因引发的复苏性SCA病例无一存活。
综上所述,在这项为期4年的全旧金山范围的OHCA研究中,只有1/3的患者是突发的,其中1/2复苏后住院,1/5活着出院。可根据心律失常原因预测生存率,近一半的死亡病例是非心律失常原因,表明SCA幸存者不等同于SCD病例。因此,早期识别非心律失常性SCA,如神经系统紧急情况,或可提高OHCA患者的生存率。
原始出处:
Ricceri Santo,Salazar James W,Vu Andrew A et al. Factors Predisposing to Survival After Resuscitation for Sudden Cardiac Arrest.[J] .J Am Coll Cardiol, 2021, 77: 2353-2362.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言















#JACC#
0
#患者生存#
44
#生存率#
35
#复苏#
36
#ACC#
32
#抢救#
37