Cardiovasc Diabetol:多因素干预对高危糖尿病肾病患者的MACE风险和死亡率的积极效益
2021-07-20 MedSci原创 MedSci原创
多因素强化治疗干预(MT)对高危DKD患者的MACE风险和死亡率有明显临床益处
糖尿病肾病(DKD)患者晚期并发症有多种可改变的风险因素,包括高血糖、高血压和血脂异常,均会增加患者不良结局的风险。DKD与非常高的心血管风险相关,这需要通过实施强化的多因素治疗方法来同时治疗这些危险因素。但是,目前多因素干预对DKD患者主要致命/非致命性心血管事件 (MACE) 的有效性研究甚少。
2型糖尿病肾病 (NID-2) 研究是一项多中心、整群随机、开放标签的临床试验,在意大利的14家糖尿病诊所中招募了395位有蛋白尿、糖尿病视网膜病变(DR),且无CV事件史的DKD患者。研究中心被随机分至主要心血管危险因素(血压<130/80 mmHg、糖化血红蛋白<7%、LDL<100 mg/dL、HDL>40/50 mg/dL[男性/女性]、总胆固醇<175 mg/dL)的标准护理组(SoC,n=188)或多因素强化治疗组(MT,n=207)。主要终点是随访阶段结束时MACE的发生率。次要终点包括主要终点和全因死亡的单一组成部分。
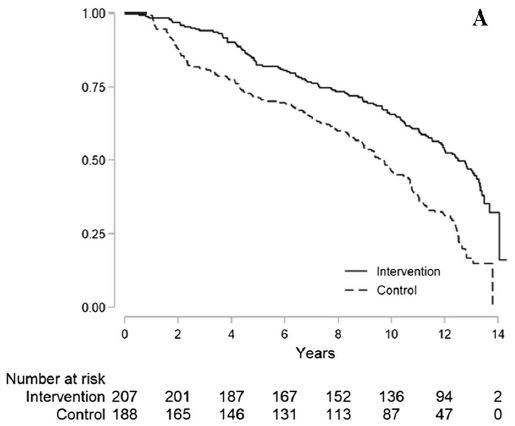
在整个研究期间两组的MACE主要终点的发生情况
在干预期结束时(MT 和 SoC 组的中位时间分别为3.84年和3.40年),MT组的目标实现率明显更高。在随访13.0年(范围12.4-13.3)期间,共记录了262例MACE(MT组 116例,SoC组 146例)。调整后的Cox共享虚弱模型显示,MT组的MACE风险降低了53%(校正HR 0.47,95%CI 0.30-0.74,p=0.001)。与此类似的,MT组的全因死亡率降低了47%(校正HR 0.53,95%CI 0.29-0.93,p=0.027)。
简而言之,多因素强化治疗干预(MT)对高危DKD患者的MACE风险和死亡率有明显临床益处。
原始出处:
Sasso Ferdinando Carlo,Pafundi Pia Clara,Simeon Vittorio et al. Efficacy and durability of multifactorial intervention on mortality and MACEs: a randomized clinical trial in type-2 diabetic kidney disease.[J] .Cardiovasc Diabetol, 2021, 20: 145. https://doi.org/10.1186/s12933-021-01343-1
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#DIA#
37
#MAC#
35
#肾病患者#
30
#ACE#
35
#BET#
28
#ASC#
36
#MACE#
35
学习了
66
谢谢MedSci提供最新的资讯
63