JAMA Cardiol:不健康的饮食可加速克隆性造血以及不良心血管事件发生发展
2021-07-04 MedSci原创 MedSci原创
随着年龄的增长,人体造血干细胞的DNA出现基因突变或拼写错误,而绝大多数的突变对造血干细胞功能没有影响,也不会诱发疾病。
随着年龄的增长,人体造血干细胞的DNA出现基因突变或拼写错误,而绝大多数的突变对造血干细胞功能没有影响,也不会诱发疾病。然而,在有些病例里,基因改变赋予特定的造血干细胞竞争优势,从而使它们有能力不成比例地扩增。称之为意义未明的克隆性造血(CHIP)。

pixabay
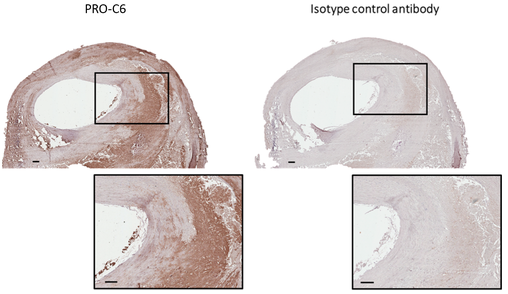
多项独立的研究已表明,克隆性造血往往与动脉粥样硬化和心血管疾病相伴而生。自发现以来,这种令人惊讶的关联一直受到临床医生和科学家们的强烈关注。由于CHIP的遗传风险很低,那么饮食质量是否与其相关?
近日,发表在JAMA Cardiol探索了饮食质量与 CHIP 患病率之间的关联。结果显示,不健康的饮食质量可能与较高的CHIP患病率和较高的不良心血管事件和死亡率有关。
在这项回顾性研究中,研究人员使用了2006年到2020年英国生物银行数据,包含年龄在40到70岁的44111名参与者,所有参与者在基线时均无冠状动脉疾病或血液肿瘤。饮食质量分为健康和不健康元素。健康元素的摄入量(水果和蔬菜等)明显高于所有调查回复的中位数;不健康元素的摄入量(红肉、加工食品和加盐)高于中位数,则饮食质量被归类为不健康的。如果健康元素的摄入量高于中位数,而不健康元素的摄入量低于中位数,则饮食被列为健康饮食。CHIP的存在是通过血液DNA全外显子组测序的数据来检测的。
结果显示,44111名参与者,平均年龄为56.3岁,在24507名女性中,2271名(5.1%)列为不健康饮食,38 552名(87.4%)为中等的饮食,3288名(7.5%)为健康饮食。共有2507人(5.7%)有CHIP,CHIP的流行率随着饮食质量的改善而下降,从不健康(2271名参与者中的162人)到中等(38552名参与者中的2177人)到健康(3288名参与者中的168人;P=0.003)。
与没有CHIP的中等饮食的人相比,在中位数10年的随访期间,不健康饮食的CHIP患者(危险比[HR],1.52;95%CI,1.04-2.22)和健康饮食的CHIP患者(HR,0.99;95%CI,0.62-1.58)的心血管事件发生率逐渐下降。
综上,不健康的饮食习惯可能与CHIP的发展以及不良心血管事件和死亡的风险增加有关。未来,需要并进一步阐明了心血管疾病与CHIP之间的相互作用。
原始出处
Romit Bhattacharya, MD1,2,3; Seyedeh Maryam Zekavat, BS2,4,5; Md Mesbah Uddin, PhD2,4; et al.Association of Diet Quality With Prevalence of Clonal Hematopoiesis and Adverse Cardiovascular Events.JAMA Cardiol. Published online June 9, 2021. doi:10.1001/jamacardio.2021.1678
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#Cardiol#
34
#克隆#
29
#发生发展#
42
#血管事件#
32
#克隆性造血#
42
#造血#
24
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
50
有用
55