JAMA Surg:病人为中心的术后疼痛管理用于颈部内分泌术后止痛
2021-09-14 MedSci原创 MedSci原创
在颈部内分泌手术后,以病人为中心的术后疼痛管理手段可减少阿片类处方量,同时不会增加患者术后疼痛负担。

阿片类药物不当使用的风险极高。有研究称,5%-10%的患者在围手术期后持续使用阿片类药物。过去,许多甲状腺和甲状旁腺手术后存在阿片类止痛药过度使用的情况。近日研究人员考察了根据患者需求的阿片类止痛方案在颈部内分泌手术止痛管理中的应用前景。

总计102名接受门诊颈部内分泌手术的成年患者参与研究,随机分为术后选择性止痛治疗(POINT组)组或常规止痛组(对照组)。POINT组患者接受在围手术期接受术后疼痛管理咨询,仅在患者要求时才服用阿片类药物。术后7日内,对患者进行术后疼痛评分(0-10),并记录阿片类药物使用情况。研究的主要结果是术后第7天的日峰值疼痛评分。
POINT组包含48名患者,对照组包含54名。其中79例患者(77.5%)为女性,平均年龄为52岁。对照组总计服用了550片阿片药物,POINT组230片(23名患者,47.9%)。术后第1周,POINT组17例患者(35.4%)报告服用了阿片类药物,而对照组患者为27例(50.0%)。对照组的门诊疼痛峰值中位评分为6分,而POINT组也为6分。在多变量分析中,既往麻醉药物使用史患者选择阿片处方的可能性增加7.5倍,服用阿片类药物的可能性高4.8倍。较高的体重指数(OR=1.11)和最高住院术后疼痛评分(OR=1.24)也与阿片类药物使用相关。
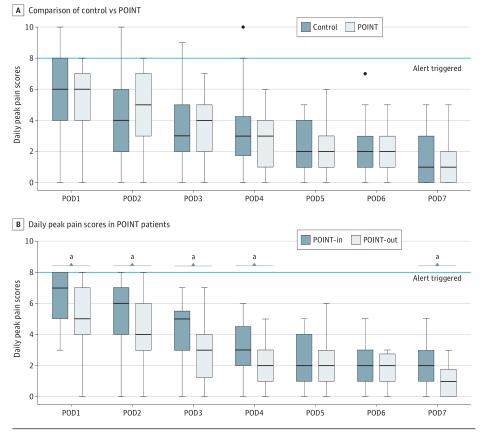
组间术后疼痛评分差异
研究认为,在颈部内分泌手术后,以病人为中心的术后疼痛管理手段可减少阿片类处方量,同时不会增加患者术后疼痛负担。
原始出处:
Catherine Y. Zhu et al. Patient-Centered Decision-making for Postoperative Narcotic-Free Endocrine Surgery A Randomized Clinical Trial. JAMA Surg. September 8,2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#分泌#
0
#疼痛管理#
42
#止痛#
58
#颈部#
44
学习#学习#
66
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
61