JAHA:心肌梗塞后射血分数大于35%的患者心脏骤停的预测因素
2021-07-14 MedSci原创 MedSci原创
射血分数(EF)降低的患者心肌梗塞(MI)后心脏骤停(SCA)风险增加。MI后EF>35%的患者年度SCA风险较大。
射血分数(EF)降低的患者心肌梗塞(MI)后心脏骤停(SCA)风险增加。然而,对于MI后EF>35%的患者SCA的危险因素知之甚少。

近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,研究人员使用2008年至2017年期间电子健康记录数据集,确定了肌钙蛋白升高的MI患者,这些患者MI后EF>35%,并接受了冠状动脉造影。该研究的主要结局是MI后1年内的SCA。该数据库通过随机选择分为推导(70%)和验证(30%)队列。Cox比例风险回归用于生成和验证风险预测模型。
 在31286名MI患者(中位年龄为64.1岁;39%为女性;87%为白人)中,499名患者在MI后1年内经历了SCA(估计概率为1.8%)。
在31286名MI患者(中位年龄为64.1岁;39%为女性;87%为白人)中,499名患者在MI后1年内经历了SCA(估计概率为1.8%)。
 MI后1年内发生SCA的预测因子
MI后1年内发生SCA的预测因子
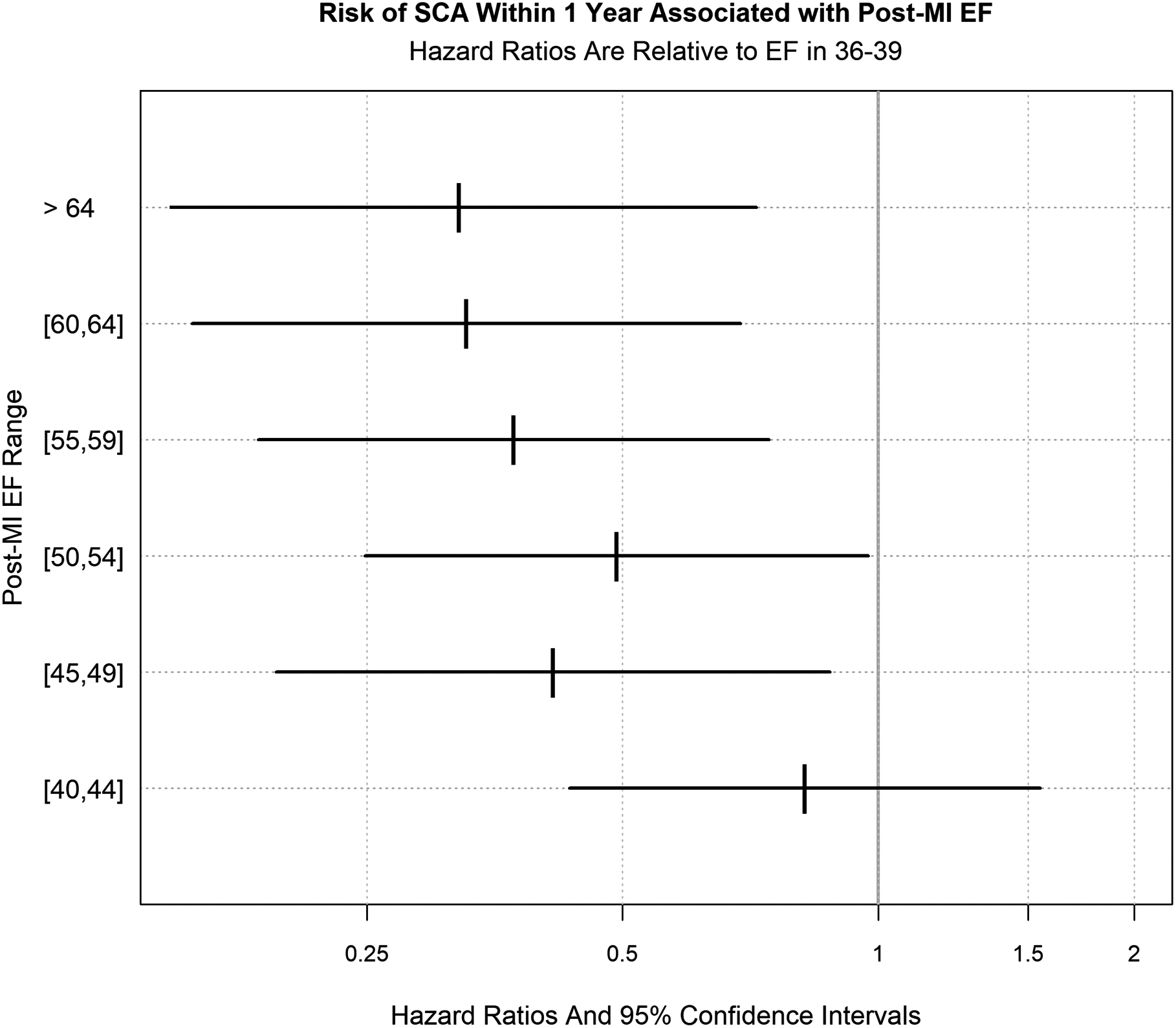
MI时未进行血运重建、MI后EF<50%、黑人、肾功能衰竭、慢性阻塞性肺疾病、接受抗心律失常治疗和未接受β受体阻滞剂治疗是SCA的独立预测因素。由这些变量组成的多变量模型可预测SCA风险(C统计量为0.73)。基于该模型,SCA的估计年概率在风险最高四分位数患者中为4.4%(95%CI为3.9-4.9),而在最低四分位数患者中为0.6%(95%CI为0.4-0.8)。
由此可见,MI后EF>35%的患者年度SCA风险较大。由急性冠状动脉血运重建、EF、种族、肾功能衰竭、慢性阻塞性肺疾病、抗心律失常治疗和β受体阻滞剂治疗组成的风险模型可以识别SCA风险较高的患者,这些患者可能受益于进一步的风险分层和更密切的监测。
原始出处:
Selçuk Adabag.et al.Predictors of Sudden Cardiac Arrest Among Patients With Post‐Myocardial Infarction Ejection Fraction Greater Than 35%.J AM HEART ASSOC.2021.https://www.ahajournals.org/doi/10.1161/JAHA.121.020993
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











学习了
39
学习了
64
#预测因素#
39
#AHA#
42
。。。。。。。。
62
,
55
,
54