Crit Care:非急性呼吸窘迫综合征患者较高和较低呼气末正压对比分析
2021-07-15 MedSci原创 MedSci原创
在这项RCT荟萃分析中,与较低PEEP相比,较高PEEP与接受有创机械通气的非ARDS患者死亡率无关。需要进一步的大型高质量RCT来证实这些结果。
近日,危重病医学领域权威杂志Critical Care上发表了一篇研究文章,研究人员对评估了接受因急性呼吸窘迫综合征 (ARDS) 以外的原因进行有创机械通气的重症监护病房 (ICU) 患者较高呼气末正压(PEEP)与住院死亡率之间关联的随机对照试验 (RCT) 进行了系统回顾和荟萃分析,并与较低呼气末正压(PEEP)进行比较。

研究人员对MEDLINE、EMBASE、Scopus、Cochrane Central Register of Controlled Trials、CINAHL和Web of Science电子数据库进行了检索,没有语言限制,检索时间从数据库成立到2021年6月16日。此外,研究人员还检索了在研数据库和灰色文献。
研究人员确定了22项比较了较高PEEP(1007名患者)和较低PEEP(991名患者)的RCT(2225名患者)。未观察到较高PEEP与住院死亡率之间存在的统计学显著的关联(风险比为1.02,95%置信区间为0.89-1.16;I2=0%,p=0.62;证据质量低)。
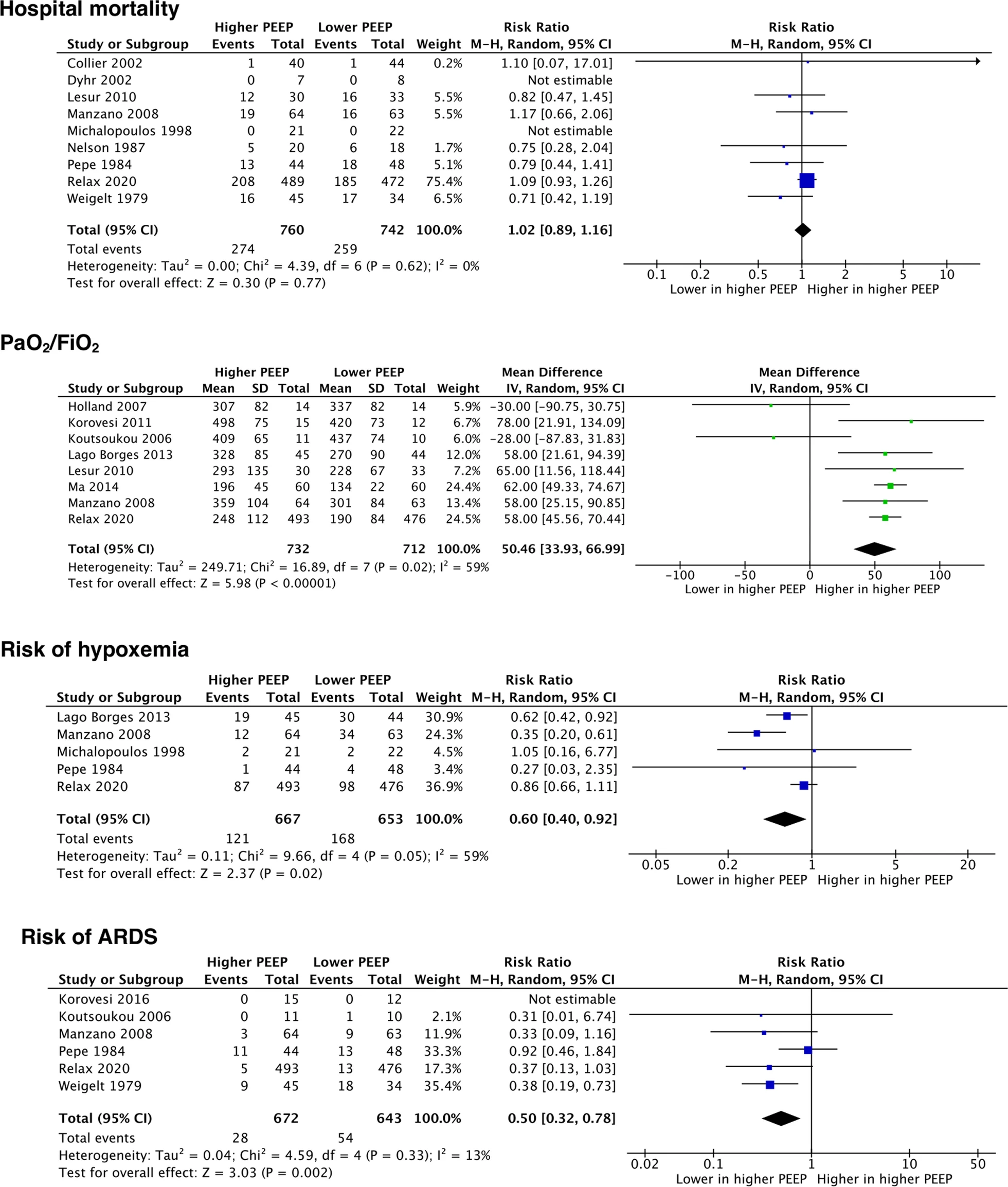 主要结局和主要次局森林图
主要结局和主要次局森林图
在次要结局中,较高的PEEP与更好的氧合、较高的呼吸系统顺应性以及较低的低氧血症和ARDS发生风险相关。此外,两组之间的气压伤、低血压、通气时间、住院时间和ICU死亡率相似。
由此可见,在这项RCT荟萃分析中,与较低PEEP相比,较高PEEP与接受有创机械通气的非ARDS患者死亡率无关。需要进一步的大型高质量RCT来证实这些结果。
原始出处:
Tommaso Pettenuzzo.et al.Higher versus lower positive end-expiratory pressure in patients without acute respiratory distress syndrome: a meta-analysis of randomized controlled trials.Critical Care.2021.https://ccforum.biomedcentral.com/articles/10.1186/s13054-021-03669-4
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








学习了
56
学习
52
#综合征#
24
#呼吸窘迫#
25
学习了 谢谢
54