
多发性硬化症(MS)是一种中枢神经系统自身免疫性脱髓鞘疾病,其特点是具有广泛的异质性。根据目前的分类,多发性硬化症可表现为复发缓解型(RRMS)、原发性进展型(PPMS)和继发性进展型(SPMS)(共同进展型MS - PMS)。
有两个实体处于中枢神经系统脱髓鞘谱系的最早期阶段:临床孤立综合征(CIS)和放射学孤立综合征(RIS)。CIS是显示MS特征的疾病的第一个临床表现,不符合传播标准。RIS是MRI偶然发现的提示MS的中枢神经系统病变,没有任何可识别的临床表现。这种异质性使疾病的过程相当不可预测,可能从一种临床过程转化为另一种。由于有不同疗效的改变病情的药物(DMD),在诊断时预测疾病演变的能力对选择最佳治疗方法变得非常重要。另外,对非特异性中枢神经系统病变患者和RIS的鉴别诊断对神经科医生来说也是一个挑战,有可能造成RIS的过度诊断。
一些生物标志物解决了这些挑战。其中,MRI和寡克隆带(OCB)是MS诊断和预后评估的支柱。MRI在多发性硬化症的管理中起着关键作用,研究MRI生物标志物可以在群体层面预测预后。然而,在病人层面的预后预测仍然是难以捉摸的,并且可能受益于补充MRI的生物标志物。其他一些生物标志物已经被测试过,但除了少数例外,它们的临床相关性仍不确定。在这种情况下,对小胶质细胞活动的探究意义重大。
大量的证据支持小胶质细胞和浸润的巨噬细胞强烈地支持神经炎症、脱髓鞘和神经损伤。小胶质细胞的激活与PMS大脑的神经变性和萎缩有关,在表面正常的脑白质(normal appearing white matter, NAWM)中,小胶质细胞的激活是弥漫的。
同时,微胶质细胞的激活与PMS的疾病进展相关。小胶质细胞的活动可以通过PET成像,使用结合18kD-translocator-protein(TSPO)的放射性配体。TSPO是一种线粒体蛋白,在激活的小胶质细胞/巨噬细胞中明显上调。TSPO-PET研究中出现了有趣的数据,包括神经炎症和神经退行性疾病。关于多发性硬化症,TSPO-PET提供了关于体内骨髓活动的新见解和关于疾病预后的有希望的结果。对辐射暴露、技术挑战和成本的担忧限制了其在临床实践中的可能应用,强调需要更方便的骨髓生物标志物。
微囊泡(MVs)是不同类型细胞(包括骨髓细胞)在生物流体中释放的细胞外囊泡。 意大利IRCCS San Raffaele Scientific Institute的Stefano Gelibter等人,证明了在人类和啮齿动物CSF中检测骨髓类MVs的可能性,将小胶质细胞激活/巨噬细胞浸润与MVs的产生联系起来。他们提出CSF髓系MVs是体内小胶质细胞/巨噬细胞激活的一个标志物。
他们纳入:诊断为神经炎症、神经退行性疾病或无神经系统疾病的601名出院患者。用流式细胞仪测量新鲜CSF中Ib4+事件的骨髓微囊泡。在诊断时(所有患者)和随访期间(n=176)收集了临床、人口学和MRI数据。
与神经退行性疾病和对照组相比,神经炎症患者的CSF骨髓微泡升高了。在多发性硬化症中,微囊泡在有MRI疾病活动的患者中较高,其浓度随着病灶数目的增加而增加(P<0.0001)。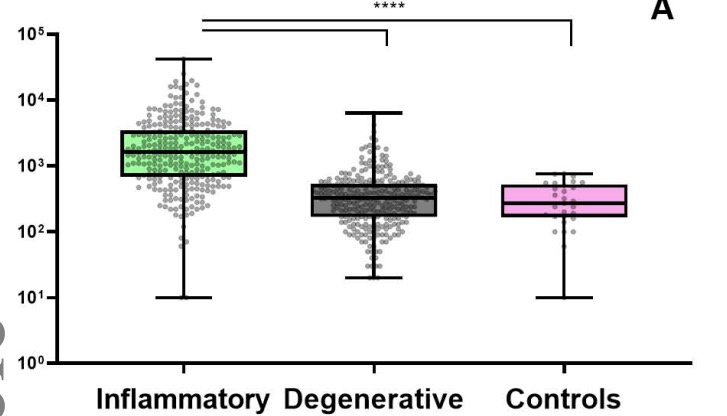
在诊断前的一个月和一年中,疾病活动较高的患者CSF骨髓微囊泡也较高。
微囊泡能很好地区分复发缓解组和对照组(ROC曲线,AUC=0.939,P<0.0001)以及放射学上的孤立综合征和非特异性脑病变(0.942,P<0.0001)。
此外,微泡是复发缓解组和进展组预后的独立预测因素。一旦校正了标准临床使用的预后因素,微泡可独立预测复发缓解期患者的未来疾病活动(HR=1.967,CI95% 1.147-3.372)。在进展期组,微泡是独立预测残疾累积的因素(HR=10.767,CI95% 1.335-86.812)。
这个研究证实了,CSF骨髓微泡是体内神经炎症和小胶质/巨噬细胞活动的一个有临床意义的生物标志物。这些发现可能支持在临床实践中用于诊断工作和预后评估。
原文出处:
Gelibter S, Pisa M, Croese T, Finardi A, Mandelli A, Sangalli F, Colombo B, Martinelli V, Comi G, Filippi M, Furlan R. Spinal fluid myeloid microvesicles predict disease course in multiple sclerosis. Ann Neurol. 2021 Jul 3. doi: 10.1002/ana.26154. Epub ahead of print. PMID: 34216397.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#多发性#
24
#Neurol#
32
#微泡#
28
学习了 谢谢
72
学习了,谢谢分享
64