European Radiology:微波消融,为无法手术的I期非小细胞肺癌患者带来希望!
2022-06-20 shaosai MedSci原创
热消融主要包括射频消融(RFA)、微波消融(MWA)、冷冻消融和不可逆电穿孔。
现阶段,手术切除仍然是早期NSCLC(非小细胞肺癌)治疗的基本术式。对于可行手术的早期NSCLC患者来说,肺切除是治疗的金标准,据报道5年生存率在60-80%之间。然而,大约有20%的患者不符合手术条件,这些患者的5年总生存率(OS)很低(从6%到14%不等)。
近年来,立体定向体外放射治疗(SBRT)和热消融在非手术早期NSCLCs的局部控制和长期生存方面取得了发展。多项前瞻性临床试验报告显示,SBRT在1年内的局部控制率至少为90%,3年内为80%以上,且毒副作用轻微。作为一种非电离辐射,热消融扩大了手术风险高的I期NSCLCs的治疗选择。
热消融主要包括射频消融(RFA)、微波消融(MWA)、冷冻消融和不可逆电穿孔。直到最近,试图评估热消融治疗I期NSCLCs的疗效和安全性的前瞻性临床试验还十分有限。2015年,涉及51例IA期NSCLCs的前瞻性、意向性治疗、多中心ACOSOG Z4033(Alliance)试验报告了2年OS率为69.8%,局部无复发率为59.8%。另一项前瞻性多中心II期试验报告,32名IA期NSCLC患者经RFA治疗后,3年OS率为58.3%。然而,关于MWA治疗早期NSCLCs的研究相对较少。
近日,发表在European Radiology杂志的一项研究评估了MWA对不能手术的I期NSCLC患者的临床效果和耐受性,为I期NSCLC患者提供了新的术式选择和更好的预后。
本研究于2011年2月-2016年3月对纳入研究的经组织学证明的临床I期NSCLC患者进行了CT引导下的MWA治疗,并进行了回顾性分析。主要终点是总生存率(OS),次要终点包括无病生存(DFS)、癌症特异性生存(CSS)和并发症。
共有105名患者接受了MWA手术,涉及105个病灶。平均年龄为70.7岁(范围:40-86岁),所有病灶的平均直径为2.40厘米(范围:0.9-4.0厘米)。腺癌是最常见的组织学类型(77,73.3%),其次是鳞状细胞癌(21,20%)和未定义的NSCLC(7,6.7%)。中位随访时间为54.8个月,中位DFS为36.0个月,1年、3年和5年DFS率分别为89.5%、49.4%和42.7%。中位CSS和OS分别为89.8和64.2个月。1年的OS率为99%,3年为75.6%,5年为54.1%,而CSS率分别为99%、78.9%和60.9%。IB期病变患者的DFS(22.3个月与未确定,HR:11.5,95%CI:5.85-22.40)和OS(37.3与89.8个月,HR:8.64,95%CI:4.49-16.60)明显短于IA期疾病。
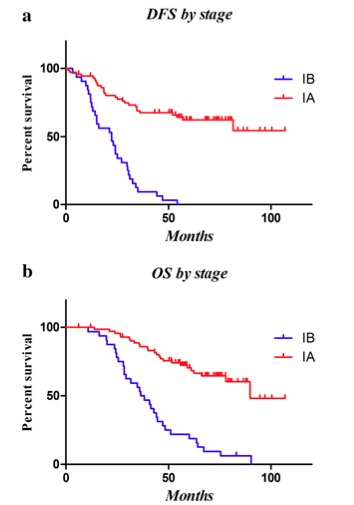
图 按阶段划分的DFS曲线:IB期患者的DFS明显短于IA期患者(22.3个月vs未确定,HR:11.5,95%CI:5.85-22.40)。 b按阶段划分的OS曲线:IB期vs IA期(37.3个月对89.8个月,HR:8.64,95%CI:4.49-16.60)
本研究为探讨MWA治疗医学上无法手术的I期NSCLC患者的最大研究之一。本研究表明,对于不适合手术切除的I期NSCLC患者来说,MWA是一种安全、有效的治愈性术式选择。
原文出处:
Yang Ni,Guanghui Huang,Xia Yang,et al.Microwave ablation treatment for medically inoperable stage I non-small cell lung cancers: long-term results.DOI:10.1007/s00330-022-08615-8.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#非小细胞#
67
#肺癌患者#
60
好
40
#PE#
53
#消融#
65
#非小细胞肺癌患者#
61