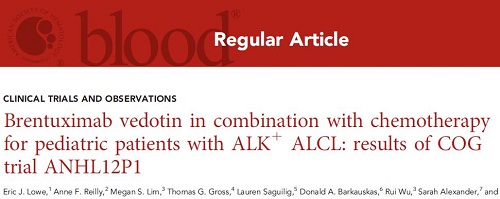
Blood:Brentuximab vedotin联合化疗治疗ALK+间变性大细胞淋巴瘤
2021-07-04 Nebula MedSci原创
与仅使用常规化疗相比,加入本妥昔单抗可改善ALK+间变性大细胞淋巴瘤患儿的OS和EFS
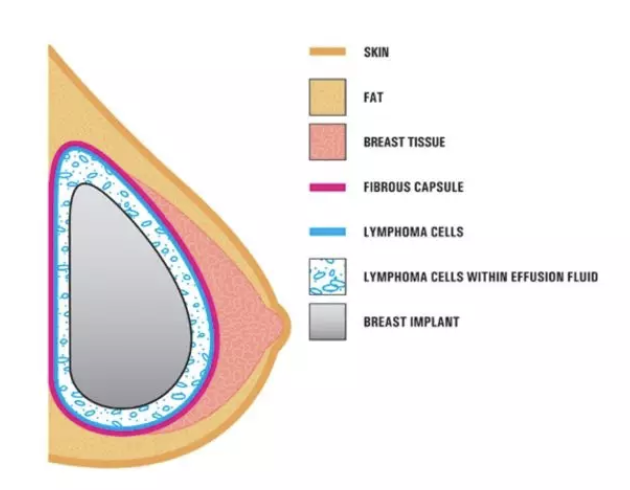
大约 30% 的间变性大细胞淋巴瘤 (ALCL) 儿科患者会复发。虽然brentuximab vedotin(本妥昔单抗) 在 ALCL 中表现出优异的活性,但尚未用于新确诊的患者。儿童肿瘤学组 (COG) 试验 ANHL12P1 确定了本妥昔单抗联合化疗对新确诊的非局部间变性大细胞淋巴瘤激酶 (ALK)+/CD30+ ALCL患儿的毒性和疗效。
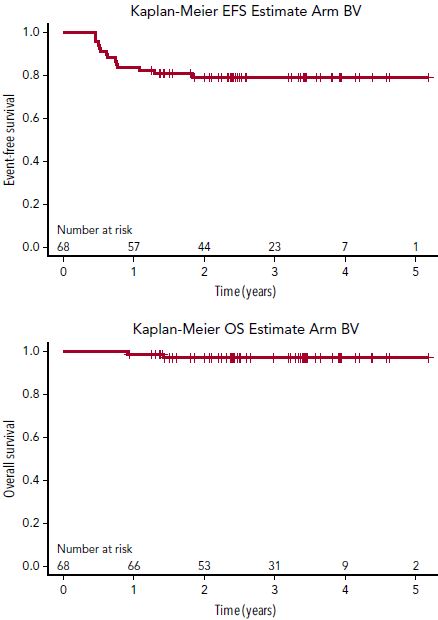
从2013年至2017年期间,该试验共招募了68位ALK+ALCL患儿,均接受了本妥昔单抗治疗。所有患儿都接受5天的前期化疗,然后进行6个疗程的化疗:每个疗程的第1天予以本妥昔单抗。
在67位可进行毒性评估的患儿中,66位完成了6个疗程的化疗,共399个可评估的疗程。无毒性相关死亡病例、无进展性多灶性白质脑病综合征病例,无3/4级神经病变病例。
EFS和OS
2年无事件生存率(EFS)为79.1%(95%CI 67.2-87.1)。2年总生存率(OS)为97.0%(95%CI 88.1-99.2)。14位患儿发生了复发。其中11位(79%)是在确诊10个月内复发的;只有1位(1.5%)患儿是在治疗期间复发的。
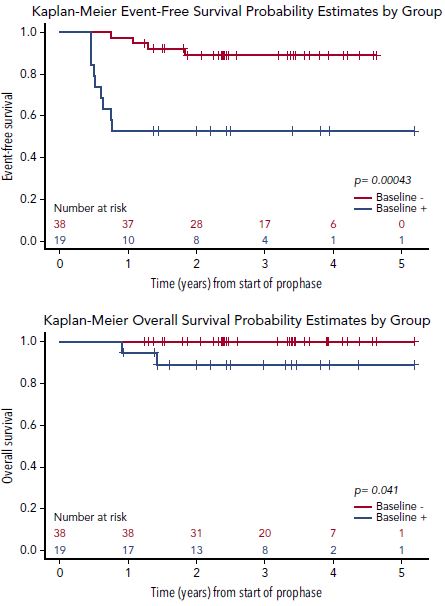
基线NPM-ALK阳性(+)或阴性(-)的患儿的EFS和OS
基线 NPM-ALK 的定量逆转录聚合酶链反应提示,NPM-ALK对EFS具有一定预测价值(p=0.0004)。
总体上,在标准化疗中加入本妥昔单抗不会增加明显的毒性或改变所需的疗程间隔,而且可预防治疗期间病情复发,与仅使用常规化疗相比,加入本妥昔单抗后的OS 和 EFS也具有一定优势。
原始出处:
Eric J. Lowe, et al. Brentuximab vedotin in combination with chemotherapy for pediatric patients with ALK+ ALCL: results of COG trial ANHL12P1. Blood (2021) 137 (26): 3595–3603.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#ALK+#
41
#细胞淋巴瘤#
40
#mAb#
0
受益匪浅
47
已读,真是受益匪浅呀。
49
#联合化疗#
46
#Brentuximab#
42
#变性#
26
#vedotin#
42
实用
51