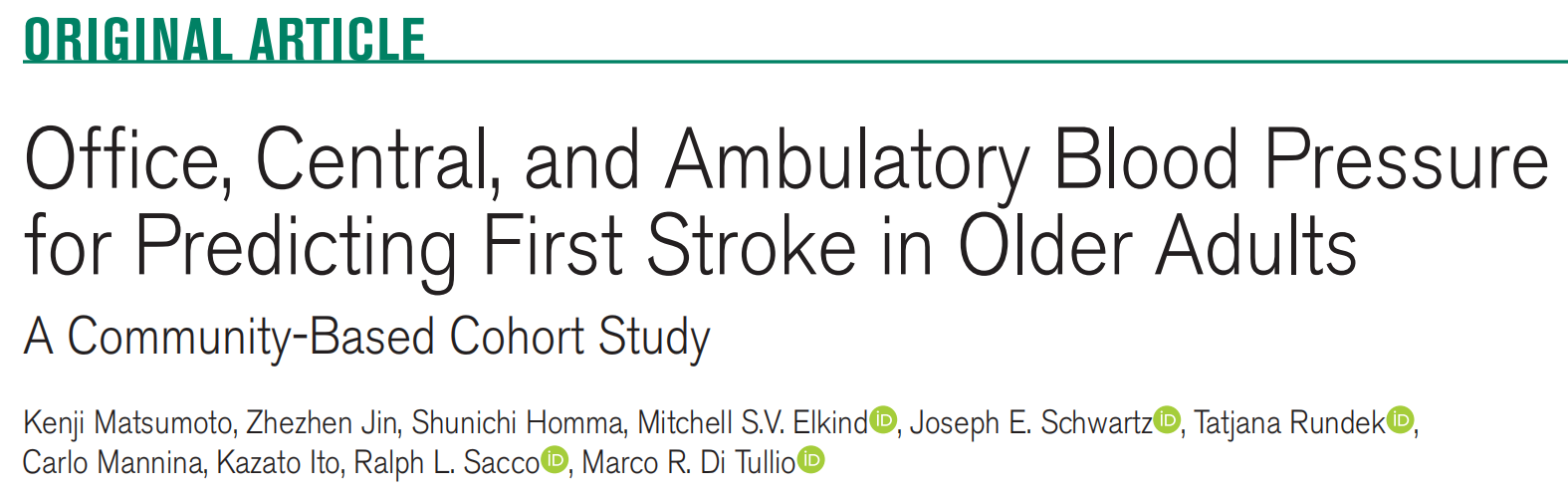
Hypertension:诊室、中心和动态血压可预测老年人首次卒中
2021-07-16 MedSci原创 MedSci原创
在以老年人群为主的队列中,诊室舒张压与卒中发生的相关性较弱;中心血压变量不能预测卒中。然而,在多变量竞争风险分析中,动态收缩压和舒张压值都与卒中显著相关。此外,动态舒张压比动态收缩压能更好地预测卒中。
高血压是卒中最常见且可改变的危险因素。诊室血压(BP)测量在确定高血压对卒中的影响方面可能存在局限性。

近日,心血管权威杂志Hypertension上发表了一篇研究文章,研究人员主要基于老年人群的前瞻性队列比较了诊室、中心和动态血压测量在卒中风险预测方面的价值。
 心血管异常和脑损伤(CABL)研究的参与者(n=816;平均年龄为70.8±9.0岁;39.8%占男性)接受了桡动脉血压测量以获得中心血压和24小时动态血压监测结果。
心血管异常和脑损伤(CABL)研究的参与者(n=816;平均年龄为70.8±9.0岁;39.8%占男性)接受了桡动脉血压测量以获得中心血压和24小时动态血压监测结果。
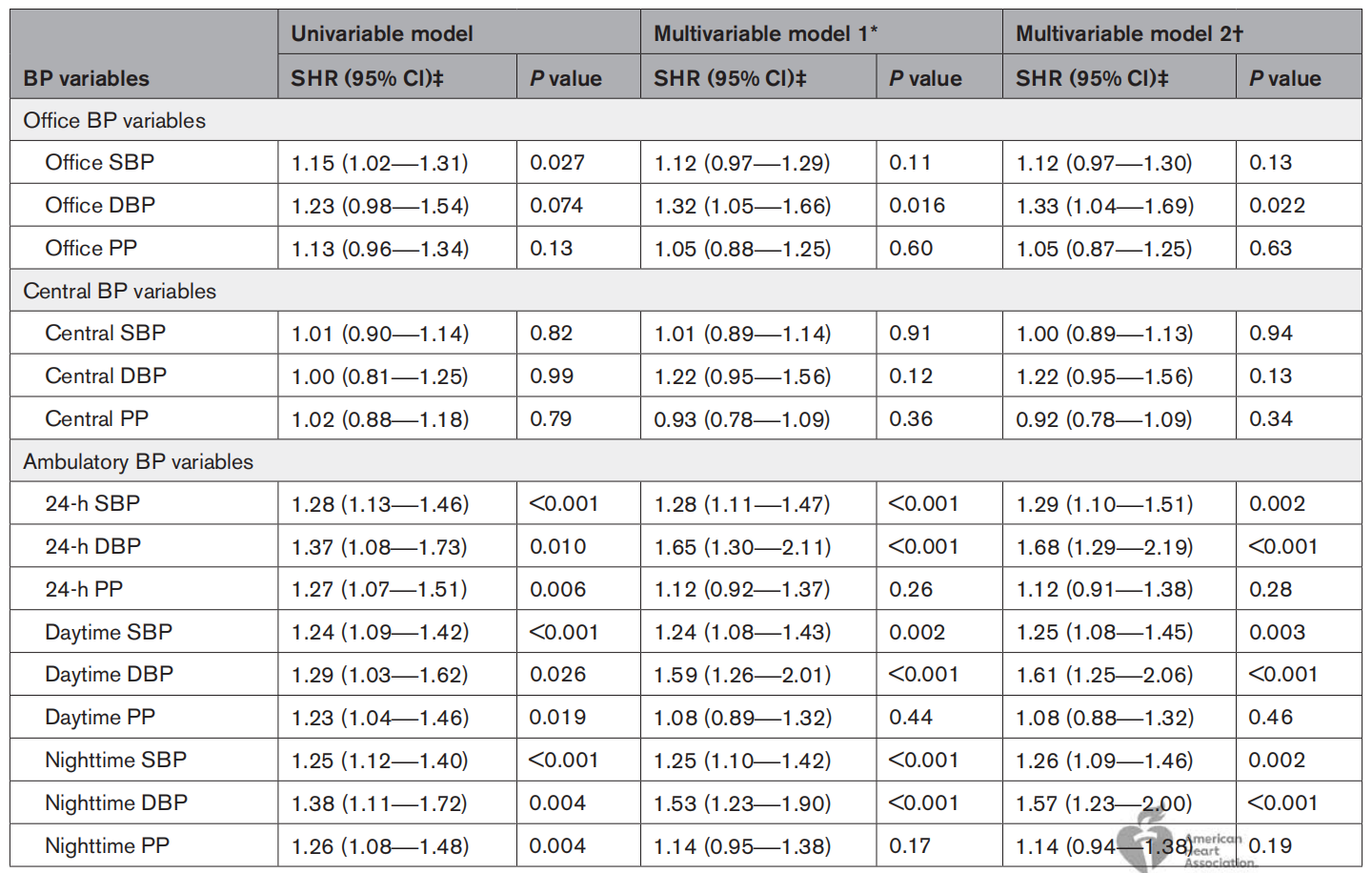 在9.6±3.1年的随访期间,76名参与者(9.3%)发生了卒中。在诊室血压变量中,多变量竞争风险模型中只有舒张压与卒中相关(P=0.016)。没有一个中心血压变量与卒中之间存在显著的关联。相反,在调整临床混杂因素后,所有动态收缩压和舒张压变量均与卒中显著相关(所有P<0.005)。在一个额外的多变量竞争风险模型中,纳入了同一天同一时间获得的动态收缩压和舒张压值,在24小时、白天和夜间期间,舒张压与卒中的相关性比收缩压更密切(所有P<0.05 )。
在9.6±3.1年的随访期间,76名参与者(9.3%)发生了卒中。在诊室血压变量中,多变量竞争风险模型中只有舒张压与卒中相关(P=0.016)。没有一个中心血压变量与卒中之间存在显著的关联。相反,在调整临床混杂因素后,所有动态收缩压和舒张压变量均与卒中显著相关(所有P<0.005)。在一个额外的多变量竞争风险模型中,纳入了同一天同一时间获得的动态收缩压和舒张压值,在24小时、白天和夜间期间,舒张压与卒中的相关性比收缩压更密切(所有P<0.05 )。
由此可见,在以老年人群为主的队列中,诊室舒张压与卒中发生的相关性较弱;中心血压变量不能预测卒中。然而,在多变量竞争风险分析中,动态收缩压和舒张压值都与卒中显著相关。此外,动态舒张压比动态收缩压能更好地预测卒中。
原始出处:
Kenji Matsumoto.et al.Office, Central, and Ambulatory Blood Pressure for Predicting First Stroke in Older Adults: A Community-Based Cohort Study.Hypertension.2021.https://www.ahajournals.org/doi/abs/10.1161/HYPERTENSIONAHA.121.17308
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#PE#
37
#TENS#
35
#Hypertension#
42
#动态血压#
48
卒中虽然是临床上常见病,溶栓,取栓等血管内治疗也很成熟,但是仍然有很多未知问题有待认知!
51
涨知识了👍👍👍
65
学习
63
学习了
65