16岁少年全身雀斑且血压升高 病因很罕见
2018-07-19 蔡军 刘力生 孙宁玲 吴海英 中国高血压疑难病例荟萃
16岁青少年,9年前出现全身皮肤雀斑,且逐渐增多、增大,以腋下为著。6年前体检发现血压中度升高,服用氨氯地平+赖诺普利,血压可达标。4年前曾主住院检查,排除了嗜铬细胞瘤。半年前起,血压重度升高。本次住院,发现病因竟异常罕见。
16岁青少年,9年前出现全身皮肤雀斑,且逐渐增多、增大,以腋下为著。6年前体检发现血压中度升高,服用氨氯地平+赖诺普利,血压可达标。4年前曾主住院检查,排除了嗜铬细胞瘤。半年前起,血压重度升高。本次住院,发现病因竟异常罕见。
病史摘要
患者16岁,男性,9年前出现全身皮肤雀斑,且逐渐增多、增大,以腋下为著。面颊、胸部、背部、大腿等处出现皮下团块,软,无痛。6年前体检发现血压中度升高,服用氨氯地平+赖诺普利,血压可达标。4年前曾在我院内分泌科住院,查MN、NMN及肾上腺CT均正常,排除嗜铬细胞瘤;双肾GFR及肾脏大小正常、对称,腹主动脉CTA排除了肾动脉狭窄,提示腹腔干起始部轻度狭窄。半年前起,血压重度升高,服用四联降压药物(托拉塞米+氨氯地平+美托洛尔+可乐定),血压140/90mmHg左右。
图26-1患者父亲的皮肤病变临床表现
体格检查
身.166cm,体.66kg。全身皮肤散在牛奶咖啡斑,皮下有大小不等的软组织团块,最大3cm×4cm,质软,无压痛(图26-2)。左上肢血压148/98mmHg,右上肢血压150/96mmHg,左下肢血压158/106mmHg,右下肢血压156/104mmHg。颈侧、脐周未及血管杂音;双肺呼吸音清,未及干湿啰音。心率80次/分,律齐。双侧下肢无水肿,足背动脉搏动对称。无视野缺损。四肢肌力、肌张力正常,生理反射存在,双侧巴宾斯基征阴性。
图26-2患者的皮肤病变临床表现
辅助检查
血常规、尿常规正常。肾功能:尿素氮:4.6mmol/L;肌酐:66μmol/L;尿酸336μmol/L。
双侧胫腓骨正位X线片:未见明显异常。
双肾上腺CT平扫加增强未见明显异常。
尿醛固酮16.55μg/1000ml尿。
血醛固酮:基础143.62pg/ml(29.4~161.5pg/ ml),立位468.34pg/ml(38.1~313.3pg/ml)。
血浆肾素:基础2.43ng/(ml·h)[0.10~5.50ng/ (ml·h)),立位3.92ng/(ml·h)[0.73~17.40ng/(ml·h)]。
血变肾上腺素、去甲变肾上腺素及尿儿茶酚胺:均正常。
尿皮质醇:74.40μg/1000ml.(20~90μg/24h)。
脑MR:未见占位性病变及血管瘤。
眼底检查:高血压眼底改变2级;虹膜表面有多个小结节。
GFR:左侧25.1ml/min;右.60.2ml/min。
肾脏大小:左侧98mm×48mm;右侧109mm× 49mm。
肾动脉CTA:左肾动脉主干远程局部(黄箭)、左肾动脉前支一级分支起始部(红箭)重度狭窄(图26-3)。
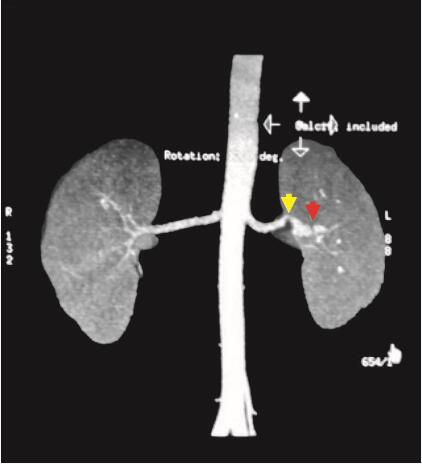
图26-3 肾动脉CTA:左肾动脉主干远程局部(黄箭)、左肾动脉前支一级分支起始部(红箭)重度狭窄
动态血压监测:24小时平均血压156/97mmHg, HR63次/分,白天平均血压161/101mmHg,HR66次/分,夜间平均血压147/89mmHg,HR57 次/分。
入院诊断
神经纤维瘤(neurofibromatosis,NF)Ⅰ型;继发性高血压(左肾动脉狭窄)
诊治经过与诊疗思路
1.简要治疗经过
行DSA术,术中见左肾动脉中段80%狭窄,多支一级分支开口处狭窄。行左肾动脉狭窄球囊扩张术,术后残余狭窄小于30%,血流通畅。术后血压明显改善:24小时平均血压136/78mmHg,HR67次/分,白天平均血压142/83mmHg,HR71次/分,夜间平均血压125/67mmHg,HR58次/分。
2. 诊疗思路
神经纤维瘤病(NF)是一种渐进性、可侵害全身各系统的常染色体显性遗传性疾病,分为.种类型,Ⅰ型神经纤维瘤病最多见,又称为冯·雷克林霍曾病,约占90%,控制基因位于常染色体17q11.2;Ⅱ型以双侧的听神经或中枢神经纤维瘤主要表现,基因位于常染色体22.长臂;其他两型很罕见,为不典型的NF。
NF的发病率约1/3000,该病在遗传学上有较大可变性,约有20%~50%的家属成员可患有相同疾患,也有不少散发病例,性别间无明显差异,其恶变率为2%。
NIH关于Ⅰ型神经纤维瘤病(NF-Ⅰ)的诊断标准:
(1)皮肤可见浅棕色的“咖啡牛奶斑”(6个或以上),直径大于5mm(青春期前)或15mm(青春期后)。
(2)两个或以上任何类型神经纤维瘤,或一个丛状神经纤维瘤。
(3)腋下或腹股沟区可见雀斑状浅棕色斑(腋窝雀斑)。
(4)视神经胶质瘤。
(5.眼部虹膜可见两个或以上色素性虹膜错构瘤(Lisch小体)。
(6)明显的骨损害,如蝶骨缺损。长骨骨皮质变薄,伴有或不伴有假性关节的形成。
(7)有一级亲属符合上述NF-Ⅰ型诊断标准者。
至少符合以上2条。
约2%NF患者可发生血管病变,其特点如下:
NF可引起全身血管病变,包括腹主动脉、髂动脉、内脏动脉(包括肠系膜上动脉、肾动脉)等。其中肾动脉最常见,近端肾动脉狭窄往往最先出现,并可引起其他动脉的狭窄,可同时发现肾动脉狭窄和腹主动脉、甲状腺动脉狭窄;其次是脑动脉的狭窄和阻塞。还可引起冠状动脉、脾动脉、回结肠动脉和内分泌器官(如胰腺、甲状腺等)动脉的病变。
NF血管病变病程缓慢,呈进行性损害。患者早期症状隐匿,可无不适症状,随病情发展,出现的临床症状视病变累及血管的部位和损伤程度而不同。病变累及肾动脉最多见,由于肾动脉狭窄,患者出现肾血管性高血压,表现为颜面部水肿、血尿和蛋白尿等。
NF导致病变的血管,按其直径和发生机制分为两类:一类为大血管,包括大动脉、颈动脉和近端肾动脉等,其病理改变为动脉壁外膜包绕神经纤维或神经节瘤组织,内膜增生,中层变薄,弹性纤维破裂,导致血管的狭窄;一类为小血管,主要指外周血管,是由于中膜层发育不全,产生狭窄或闭塞,与神经畸形无关。组织学上可见累及的血管有多发性结节生成,超显微技术下发现这些结节来源于血管壁内平滑肌。患者可同时发生这两种血管病变。
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#雀斑#
24
#血压升高#
26
很不错的病例
72
#罕见#
32
学习了,长知识
82
学习了,谢谢老师分享
76
学习
72
学习了,长知识
82