Am J Transplant:极低体重新生儿供肾双肾整块移植新术式
2018-03-22 余少杰 湘雅二院
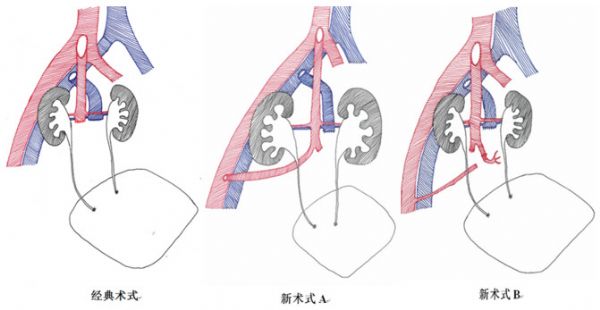
近日,中南大学湘雅二医院泌外器官移植科主任彭龙开教授带领的团队在《美国器官移植杂志》(简称AJT)发表名为《利用主动脉远端建立流出道的极低体重新生儿供肾双肾整块移植新术式》(A novel technique for en bloc kidney transplantation from infant donors with extremely low body weight by using t
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Transplant#
39
#TRA#
35
#plant#
25
认真学习了.谢谢
58
学习了.学习分享
83
阅
1